ISSN 2041-1723 (online)
Editor’s note: Keytruda was the first cancer drug approved to treat any solid tumor – anywhere in the body – that displays specific molecular characteristics. This marks
the 1st time that the FDA has approved a cancer drug based on the tumor’s molecular characteristics, regardless of its organ site.
Here are five important things to know about this landmark cancer drug:
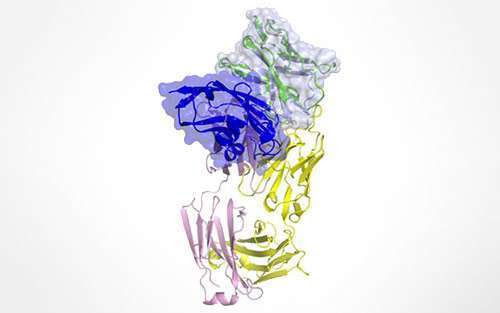
Keytruda works as an immunotherapy drug. This means that it aims to trigger a patient’s immune system to recognize and launch an attack against cancer cells. T-cells are a key immune cell type that, when activated, can destroy cancer cells as foreign invaders – but the tumor puts out signals that scare them off. Keytruda blocks those signals.“There is reason to believe that there are T-cells that recognize cancer cells,” said Dung Le, MD, associate professor of oncology at the Johns Hopkins University School of Medicine and a Pancreatic Cancer Action Network research grant recipient. “But we still have to figure out how to get them into the tumor and get them to kill cancer cells before they are turned off. With new immunotherapy agents like Keytruda, there is hope.”
Microsatellite instability (MSI) and DNA mismatch repair deficiency
are the molecular alterations that triggers a patient’s response to Keytruda.
High MSI and DNA mismatch repair deficiency result in significant accumulation of DNA damage, leading to a high number of mutated, deviant proteins within the cancer cells.
When T-cells scan the body looking for foreign invaders, the abnormal proteins expressed by cancer cells with high-MSI or mismatch repair deficiency catch the T-cells’ attention – and they can recognize and destroy the cancer cells as long as drugs like Keytruda are also present.
Keytruda is an example of precision medicine. When a patient’s treatment is based on their tumor’s molecular characteristics, it’s called precision medicine. “Every pancreatic tumor is different,” explained Cassadie Moravek, senior manager of clinical initiatives for the Pancreatic Cancer Action Network. “We strongly recommend molecular profiling of patients’ tumors to help determine the best treatment options.” Eligible pancreatic cancer patients can enroll in our Know Your Tumor® precision medicine service to determine their MSI and mismatch repair status, as well as to reveal other molecular alterations that could help inform treatment decisions.
About 1 to 3 percent of pancreatic cancer patients have high MSI or DNA mismatch repair deficiency. Overall, high MSI or mismatch repair deficiency can
be found in about 4 percent of all advanced solid tumors. “These are small numbers, but with a disease like pancreatic cancer, a drug that will work well in even a small subset of patients is still a major step forward,” said Moravek. “Being able to chip away at the disease by identifying effective treatment options for different subtypes of patients will move us toward our goal to double pancreatic cancer survival by 2020 – and beyond.”
Our PanCAN Patient Services Case Managers can help patients get molecular profiling. If you have any questions about Keytruda, how to determine your or a loved one’s MSI or mismatch repair status or any other pancreatic cancer-related topics, please contact us today.
Additional reading:
Article about Keytruda’s FDA approval
Q&A with Dr. Dung Le about Keytruda and immunotherapy
Dr. Le’s first-author Science paper about DNA mismatch repair and Keytruda
Washington Post article featuring Dr. Le

Houston Methodist Research Institute nanomedicine researchers used an implantable nanofluidic device smaller than a grain of rice to deliver immunotherapy directly into a pancreatic tumor. Credit: Houston Methodist
Implantable device, smaller than a grain of rice,
shown to shrink pancreatic tumors
by Houston Methodist
Houston Methodist nanomedicine researchers:
Have found a way to tame pancreatic cancer—one of the most aggressive and difficult to treat cancers—by delivering immunotherapy directly into the tumor with a device that is smaller than a grain of rice. In a paper recently published in Advanced Science, Houston Methodist Research Institute researchers used an implantable nanofluidic device they invented to deliver CD40 monoclonal antibodies (mAb), a promising immunotherapeutic agent, at a sustained low-dose via the nanofluidic drug-eluting seed (NDES).
The result, found in murine models, was tumor reduction at a fourfold lower dosage than traditional systemic immunotherapy treatment. “One of the most exciting findings was that even though the NDES device was only inserted in one of two tumors in the same animal model, we noted shrinkage in the tumor without the device,” said Corrine Ying Xuan Chua, Ph.D., co-corresponding author and assistant professor of nanomedicine at Houston Methodist Academic Institute.
“This means that local treatment with immunotherapy was able to activate the immune response to target other tumors. In fact, one animal model remained tumor-free for the 100-days of continued observation.” Pancreatic ductal adenocarcinoma is frequently diagnosed at advanced stages. In fact, about 85% of patients already have metastatic disease at diagnosis. Immunotherapy holds promise in treating cancers that previously
did not have good treatment options.
However, because immunotherapy is delivered throughout the entire body,
it causes many side effects that are sometimes long-lasting, if not life-long.
By focusing the delivery directly into the tumor, the body is protected from being exposed to toxic drugs and fewer side effects, essentially allowing patients undergoing treatment to have a better quality of life. “Our goal is to transform the way cancer is treated. We see this device as a viable approach to penetrating the pancreatic tumor in a minimally invasive and effective manner.
Allowing for a more focused therapy using less medication,” said Alessandro Grattoni, Ph.D., co-corresponding author and chair of the Department of Nanomedicine at Houston Methodist Research Institute.The Houston Methodist researchers are studying similar nanofluidic delivery technology on the International Space Station. Grattoni’s nanomedicine lab at Houston Methodist focuses on implantable nanofluidics-based platforms for controlled and long-term drug delivery and cell transplantation to treat chronic diseases.
It’s called a nanofluidic drug-eluting seed (NDES).
Implantable device, smaller than a grain of rice, shown to shrink pancreatic tumors…
The NDES device consists of a stainless-steel drug reservoir containing nanochannels, thus creating a membrane that allows for sustained diffusion when the drug is released. Other medical technology companies offer intratumoral drug-eluting implants for cancer therapeutics, but those are intended for shorter duration use. The Houston Methodist nanofluidic device is intended for long-term controlled and sustained release, avoiding repeated systemic treatment that often leads to adverse side effects.
Additional lab research is underway to determine the effectiveness and safety of this delivery technology, New research in mice shows promise for a potential therapy for pancreatic cancer, which can be aggressive and hard to treat.
Researchers from Houston Methodist tested a device that,
while smaller than a grain of rice, could deliver immunotherapy directly
into a pancreatic tumor. It’s called a nanofluidic drug-eluting seed (NDES).
The scientists invented the implantable device to deliver CD40 monoclonal antibodies at a sustained low dose. Tumors shrank at a dose that was four times lower than traditional systemic immunotherapy, the study authors reported. However, the findings are early, and research done in animals is often different when repeated in people. “One of the most exciting findings was that even though the NDES device was only inserted in one of two tumors in the same animal model.
We noted shrinkage in the tumor without the device,” said study co-author
Corrine Ying Xuan Chua, an assistant professor of nanomedicine at Houston Methodist Academic Institute. “This means that local treatment with immunotherapy was able to activate the immune response to target other tumors. In fact, one animal model remained tumor-free for the 100 days of continued observation,” she said in an institute news release.
By the time pancreatic ductal adenocarcinoma is typically diagnosed, it has already spread in about 85% of patients. Immunotherapy is promising for treating cancers that have lacked good treatment options. But it can cause many side effects, because it is delivered throughout the body. By delivering the treatment directly into the tumor, the body is protected from exposure to toxic drugs, according to the study.
This allows for a better quality of life during treatment.
“Our goal is to transform the way cancer is treated,” said study co-author Alessandro Grattoni, chair of nanomedicine at Houston Methodist Research Institute. “We see this device as a viable approach to penetrating the pancreatic tumor in a minimally invasive and effective manner, allowing also for a more focused therapy using less medication.”
The NDES device consists of a stainless-steel drug reservoir containing nanochannels.
Other medical technology companies offer intratumor implants for cancer therapeutics, but they are intended to be used for a shorter time. This device is intended for long-term controlled and sustained release, avoiding repeated systemic treatment. The study results were recently published online in the journal Advanced Science.
Houston Methodist Research Institute collaborators on this study include Hsuan-Chen Liu, Daniel Davila Gonzalez, Dixita Ishani Viswanath, Robin Shea Vander Pol, Shani Zakiya Saunders, Nicola Di Trani, Yitian Xu, Junjun Zheng and Shu-Hsia Chen.
New research in mice shows promise for a potential therapy for pancreatic cancer, which can be aggressive and hard to treat. Researchers from Houston Methodist tested a device that, while smaller than a grain of rice, could deliver immunotherapy directly into a pancreatic tumor. Provided by Houston Methodist
More information: Hsuan‐Chen Liu et al,
Sustained Intra tumoral Administration of Agonist CD40 Antibody Overcomes
Immunosuppressive Tumor Microenvironment in Pancreatic Cancer, Advanced Science (2023). DOI: 10.1002/advs.202206873
Journal information: Advanced Science
Read more:
Nano therapy for cancer
Drug cures rectal cancer patients in new trial.
Will this impact the current course of treatment?
Genetic mapping of cancer cells raises hope of improved treatment
The study results were recently published online in the journal Advanced Science.
Pelosi reaches $700K in gas-guzzling private jet payments despite pushing green energy
 Injections of chemotherapy drugs often fail because the pancreas is so deep within the body. (Photo: AP)
Injections of chemotherapy drugs often fail because the pancreas is so deep within the body. (Photo: AP)Washington: MIT researchers have developed a small, implantable device that delivers chemotherapy drugs directly to pancreatic tumors, and can potentially help shrink the tumors to a size where a surgeon can remove them. In a study of mice, researchers found that this approach was up to 12 times more effective than giving chemotherapy drugs by intravenous injection, which is how most pancreatic cancer patients are treated.
“It is clear there is huge potential for a device that can localise treatment at the disease site,” said Laura Indolfi, from Massachusetts Institute of Technology (MIT)’s Institute for Medical Engineering and Science (IMES). “You can implant our device to achieve a localised drug release to control tumour progression and potentially shrink (the tumour) to a size where a surgeon can remove it,” said Indolfi. This thin, flexible film could also be adapted to treat other hard-to-reach tumours, researchers said.
Injections of chemotherapy drugs often fail not only because the pancreas is so deep within the body, but also because pancreatic tumours have few blood vessels, making it harder for drugs to get in. Also, pancreatic tumours are often surrounded by a thick, fibrous coating that keeps drugs out. In hopes that getting drugs directly to the tumour site would improve treatment, the researchers engineered a flexible polymer film that is made from a polymer called PLGA, which is widely used for drug delivery and other medical applications.
The film can be rolled into a narrow tube and inserted through a catheter, so surgically implanting it is relatively simple. Once the film reaches the pancreas, it unfolds and conforms to the shape of the tumour. “Because it is very flexible it can adapt to whatever size and shape the tumour will have,” Indolfi said. Drugs are embedded into the film and then released over a preprogrammed period of time.
The film is designed so that the drug is only secreted from the side in contact with the tumour, minimising side effects on nearby organs. Researchers, including those from Massachusetts General Hospital, compared two groups of mice carrying transplanted human pancreatic tumors.
One group received the drug-delivery implant loaded with the chemotherapy drug paclitaxel, and the other received systemic injections of the same drug for four weeks, which mimics the treatment human patients usually receive.
In mice with the drug-delivery implant, tumor growth slowed,
and in some cases tumors shrank.
The localized treatment also increased the amount of necrotic tissue (dead cancer cells that are easier to remove surgically). Additionally, by acting as a physical barrier, the film was able to reduce metastasis to nearby organs. The researchers also found that after four weeks, the concentration of paclitaxel in the tumors of mice with the implanted device was five times greater than in mice that received injections.
The research was published in the journal Biomaterials.
Dr. Robert Martin & Elise Tedeschi-Stage 3 Pancreatic Cancer
BONUS: Dr Robert Martin Louisville Ky – Search (bing.com)
Whipple Surgery @ Dr Robert Martin – Bing video
Chemo FAQ | Cancer Quick Facts (solitarius.org)
Dr Robert Nagourney Long Beach Cali – Bing video
Eat Clean, Before, During After Chemo,
Chemo Sensitivity Testing – Bing video
Chemo care – Side Effects – Drug Info,









 I’m going through a pretty tough period in my life right now,
I’m going through a pretty tough period in my life right now,  Thank you Heavenly Father there’s so much to learn, if we just allow ourselves to open up to our Lord. He never forces Himself on us, He gives us free will, He promises us that He will never forsake us, He patiently waits until we’re at our weakest point if we come to Him. He will hold our hand every step of the way, even when our faith is nothing more than a mustard seed, so while we come to Him while we’re broken by a dying world, He breathes a breath of fresh air and rescues us. He Loves us know dought!!!” Amén
Thank you Heavenly Father there’s so much to learn, if we just allow ourselves to open up to our Lord. He never forces Himself on us, He gives us free will, He promises us that He will never forsake us, He patiently waits until we’re at our weakest point if we come to Him. He will hold our hand every step of the way, even when our faith is nothing more than a mustard seed, so while we come to Him while we’re broken by a dying world, He breathes a breath of fresh air and rescues us. He Loves us know dought!!!” Amén


 THE GOOD NEWS
THE GOOD NEWS

 ️
️





 Jim Watson
Jim Watson

 IVM taken by body weight with food.
IVM taken by body weight with food.  Blessings to you.
Blessings to you. 

 and could not get a doctor to prescribe it.
and could not get a doctor to prescribe it.

 God
God  Be
Be You Always
You Always 














 retiring to Trump’s neighborhood.
retiring to Trump’s neighborhood. 



