98 Percent of People with Alzheimer’s Develop This Symptom First, Study Says
Right now, more than six million Americans are living with Alzheimer’s disease (AD), a form of dementia that destroys memory and the ability to function normally. It’s the sixth leading cause of death in the United States, but how exactly it develops can be different for each person. Now, a new study has found that in those with late-onset Alzheimer’s dementia (LOAD)—meaning those in which the first symptoms appear past the age of 65—98 percent of patients develop one symptom first. Read on to find out which symptom may appear before others in late-onset cases, and how to spot it.
RELATED: This Could Be Your First Sign of Dementia Years Before Diagnosis, Study Says.
In late-onset cases, 98 percent of patients experience depression as a first symptom.
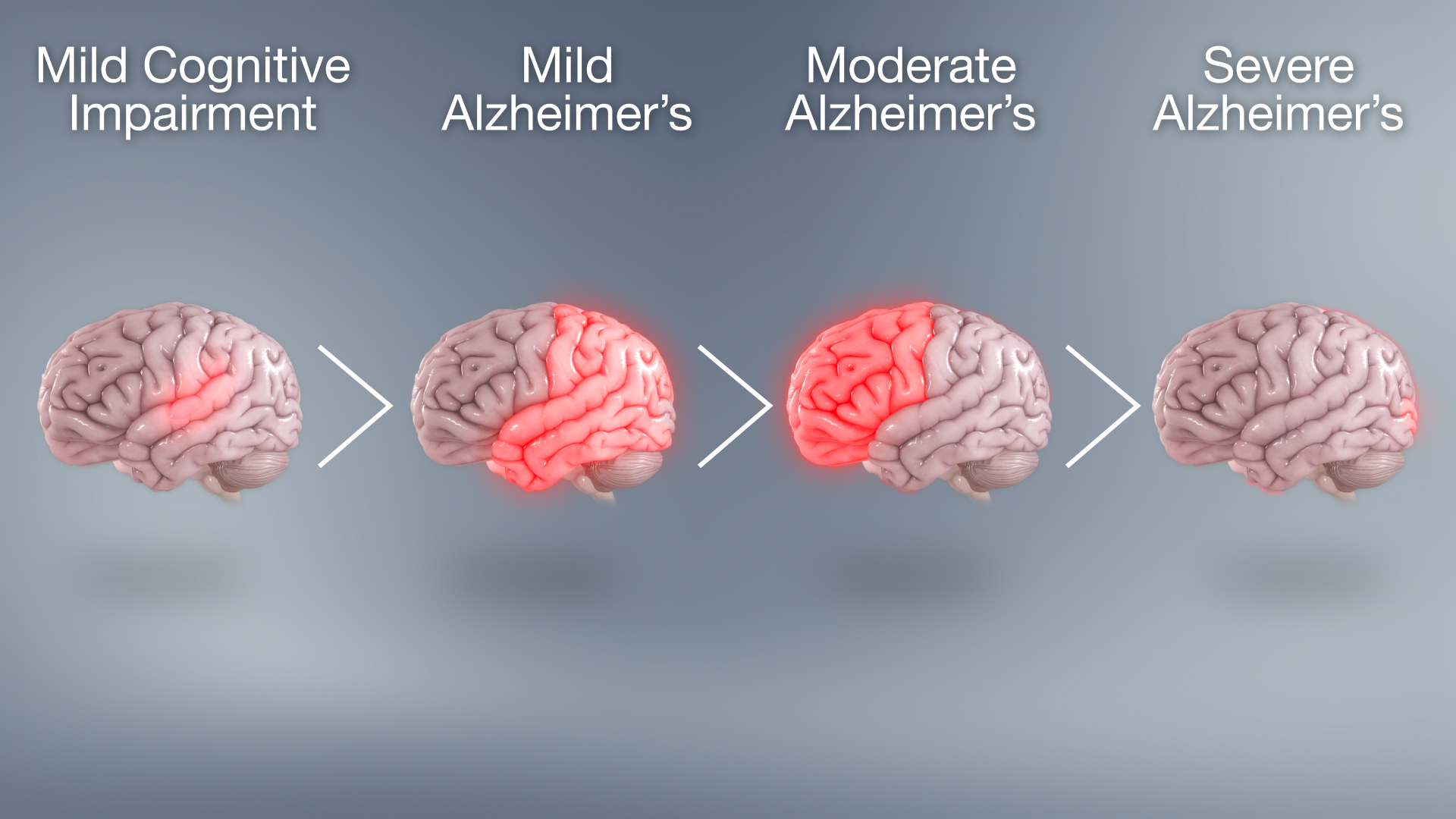
Experts have long reported that the majority of dementia cases begin with mild cognitive impairment. However, research suggests that in the case of late-onset Alzheimer’s disease—defined as cases in which the first symptoms appear after the age of 65—there’s an additional symptom that’s missing from this picture.
According to a 2017 study published in the journal BMJ Open, depression occurs as a first symptom of late-onset Alzheimer’s with nearly the exact same frequency as cognitive impairment—a fact which distinguishes it from early-onset cases of the condition. “We found that depression and cognitive impairment were the first symptoms to appear in 98.5 percent and 99.1 percent of individuals in a study with late-onset AD (LOAD) and 9 percent and 80 percent, respectively, in early-onset AD (EOAD),” the team wrote.
This data suggests that depression occurs as a compounding first symptom in the vast majority of late-onset cases of Alzheimer’s, while being relatively rare as a first symptom in early-onset cases. This is especially relevant, given that the National Institute on Aging estimates that 90 percent of Alzheimer’s cases are considered late-onset.
RELATED: This Heartburn Medication Raises Your Dementia Risk 44 Percent, Study Says.
Depression may look different in Alzheimer’s patients.
Though Alzheimer’s-related depression is considered common, it may be more challenging to spot than depression in the general population. “Identifying depression in someone with Alzheimer’s can be difficult, since dementia can cause some of the same symptoms,” explains the Alzheimer’s Association. “In addition, the cognitive impairment experienced by people with Alzheimer’s often makes it difficult for them to articulate their sadness, hopelessness, guilt, and other feelings associated with depression,” their experts say. Symptoms shared between depression and dementia include apathy, loss of interest in activities, social withdrawal, isolation, difficulty concentrating, and impaired thinking.
The organization also notes that depression associated with Alzheimer’s disease may look a bit different from depression in the general population. Depression in AD patients may be less severe, last a shorter period of time, or come and go intermittently. AD patients with depression may also be less likely to talk about or attempt suicide than other people with depression.
Targeting depression may help slow the progression of AD.
In those with Alzheimer’s, abnormal levels of brain amyloid—a naturally occurring protein—bond to form plaques that collect between neurons in the brain. This disrupts cell function, contributing to cognitive impairment, experts say. According to Harvard Health Publishing, there’s evidence to suggest that depressed individuals with abnormal levels of brain amyloid may experience quicker cognitive decline, including changes in memory and thinking.
“Our research found that even modest levels of brain amyloid deposition can impact the relationship between depression symptoms and cognitive abilities,” said Jennifer Gatchel, HMS, assistant professor of psychiatry and a geriatric psychiatrist at Mass General. “This raises the possibility that depression symptoms could be targets in clinical trials aimed at delaying the progression of Alzheimer’s disease. Further research is needed in this area,” she said.
Gatchel adds that because depression “may be among the early changes in the preclinical stages of dementia syndromes,” recognizing it could create “a clinical window of opportunity for closely monitoring at-risk individuals and for potentially introducing interventions to prevent or slow cognitive decline.”
Treatment can improve quality of life in AD patients.
Identifying depression is the first step to treating it. However, in Alzheimer’s patients, this may present its own set of challenges. “Because of the complexities involved in diagnosing depression in someone with Alzheimer’s, it may be helpful to consult a geriatric psychiatrist who specializes in recognizing and treating depression in older adults,” recommends the Alzheimer’s Association.
They add that The National Institute of Mental Health has established a separate set of guidelines for diagnosing depression in AD patients. “Although the criteria are similar to general diagnostic standards for major depression, they reduce emphasis on verbal expression and include irritability and social isolation,” their experts note.
Once diagnosed, many Alzheimer’s patients benefit from a combination of medication, counseling, and lifestyle interventions including “gradual reconnection to activities and people that bring happiness.”
Speak with your doctor today about whether screening or treatment may be right for you.
RELATED: Drinking This Makes You 3 Times More Likely to Get Dementia, Study Says.
As we age our bodily systems begins to go haywire and vitamin D is one deficiency that is common in elderly people. Because as the skin ages it has a reduced capacity to synthesize it and as you get older you become less apt to get out in the sun exposure which is necessary for the synthesis of the vital vitamin. If you have a relative with early signs of dementia you should always request a simple blood test level for vitamin D and Zinc levels (A Welsh Alternative.)
Although when your talking hereditary the ApoE gene, short for Apoliprotein E which provides instructions for making the protein (responsible for transporting cholesterol through the blood stream.) There are three different versions of genes ApoE2, E3 & E4 or in combination. Therefore, having two copies of ApoE2 increases your risk of premature vascular disease or two copies ApoE4 Alzheimer, with 62% carrying the ApoE3 genotype with a risk of neither. http://www.wellcome.ac.uk/Funding/Biomedical-science/Funded-projects/Major-initiatives/Neurodegenerative-Diseases-Initiative/WTDV027075.htm
Always remember also that as you age there is “no” substitute for a healthy diet and regular exercise. It’s important to eat good sources of B vitamins, food rich in vitamin C and Vitamin E that adds protection from free radical damage. Latest discovery in this area indicates that free radicals generated…. by compounds isolated from Alzheimer’s brain tissue can even damage parts of brain cells called acetlycholine receptors which are needed for receiving memory signals. Human Nervous System!!! Daniel Tammet: The Boy With The Incredible Mind? Kim Peek Murray, Utah… https://www.google.com/webhp?sourceid=navclient&ie=daniel+tammet
In addition, brain cell culture studies show vitamin E can protect against damage caused by amyloid proteins that accumulate abnormally in the brains of Alzheimer’s patients. It’s important to note that currrent vitamin E supplements contain alpha tocopherol, therefore, a good diet is essential to obtain gamma tocopherol. study-holds-promise-for-new-alzheimers-treatment/
Keeping physically active: there exist a connection between good cardiorespiratory fitness and preservation of the hippocampus region in the brain that’s important in memory and spatial navigation. It is also one of the first brain regions to suffer Alzheimer related damage. Also increased levels of social interaction and cognitive stimulation have been shown to be beneficial to overall cognitive levels through reducing stress levels in your everyday life.
Mentally stimulating activities helps maintain and strengthens the link amongst brain cells, as well as brain cells themselves thereby contributing to the creation of new nerve cells. Also Staying cognitively active over your lifetime may reduce the risk of Alzheimer by preventing he accumulation of Alzheimers related pathology says Susan Landau, a scientist at the Helen Willis Neuroscience Institute at University of Cal Berkeley.
Several “NEW” studies show that treating hypertension can reduce one risk for developing Alzheimer’s disease as well as other forms of cognitive impairment. While hypertension is not believed to be a cause of Alzheimer’s it can be considered a risk factor. It is thought to be partially responsible for the subcortical white matter lesions and a dysfunction of the blood brain barrier commonly found in Alzheimer’s diseased patients.
Furthermore, several other studies have begun to investigate which anti – hypertensive medications have the greatest impact upon reducing cognitive impairment. One study showed that centrally acting ACE inhibitors have the largest impact on improving cognition in patients with early stage cognitive impairment. ACE inhibitors helps remove amyloid plaque from brain tissue and thus frees it of it’s amyloid burden.
When you piece “the puzzle together“ the big picture gets brighter. While for instance in Alzheimer patients the brain has “gray matter” that consist of neurons (nerve cells), while the white matter consist of nerve fibers, as well as, glial cells which support the neurons. When you take into account “white matter disease” is damage done to the white matter by damaged blood vessels.
Apart from instances of high blood pressure, high cholesterol and smoking being the biggest factors in ischemic white matter disease of the brain. Improving these factors can reduce the risk of vascular dementia. Which is similar to Alzheimer, whereas, dementia tends to be stable for a while then suddenly gets worse, Alzheimer disease progress slowly with this being a surprising method of testing yourself cheaply.
Also remember: that Lewy body dementia is the second most common type 0f dementia after Alzheimer. It’s always important to make a diagnosis 0f LBD rather than Alzheimer’s because the treatments are different. Many medicines used with success in Alzheimer disease are useless or will worsen LBD. So it’s important to get the right diagnosis, treatment with neither showing up in a CT scan or MRI and can be a struggle finding the right diagnosis/medicine. For helpful information www.lbda.org www.alz.org http://www.nia.nih.gov/alzheimers/alzheimers-disease-research-centers http://report.nih.gov/NIHfactsheets/ViewFactSheet.aspx?csid=107http://nihseniorhealth.gov/alzheimersdisease/research/01.html http://www.nia.nih.gov/alzheimers/about-adear-center http://alzfdn.org/ eldercare.gov caregiver.org
While other popular neurodegenerative disorders…. are Epilepsy Huntington, Lou Gehrig’s (A.L.S.) , Multiple Sclerosis, Parkinson Disease with symptoms including differences in speech patterns, loss of balance and coordination, numbness or weakness in single a extremity, memory loss, difficulty in moving or swallowing, tremors, rigid muscles. With one of the best treatment centers (Cushing Neuroscience Institutes) and Can Stress Actually Kill You!
Courtney Galiano whom at 25 years old and dancing since she was three years old. Developed an electricity feeling all the way down to her toes, therefore, being diagnosed with multi sclerosis. Which is a potentially debilitating disease which the body’s immune system attacks the protective myelin sheath that covers the nerve tissue in the brain. Whereas, this damage interferes with communication between your brain, spinal cord and other parts of your body. Checkout www.gethealthystayhealthy.com for additional information….
Also April 2011, Coach Pat Summitt of The Lady Vols basketball team, in Knoxville Tennessee was diagnosed with early onset dementia. Starting her career in 1974, at the age of 22… she developed quite a reputation in her 38 years as head coach winning Eight 8 National Championships. Summitt determination remains with a mantra: keep fighting, keep living & keep making the most of everyday. Now – A – day’s she’s making an impact with the challenges of A.D. says, Dr. Ronald Petersen, the Director of Alzheimer’s Disease Research Center at the Mayo Clinic in Rochester, Minnesota by launching The Pat Summitt Foundation. http://alzheimersawareness.net/im-still-here/
The end stage of dementia is the most difficult stage for those suffering from the disease, and also for family members, caregivers, and healthcare professionals. Victims lose what is left of their intellectual and physical capabilities and become completely dependent on others. The model is still shifting in considering end stage dementia an end of life condition; experts are pushing this model in order to advocate for better pain and distress management for those suffering at their end.
What Happens
In the end stages of dementia, many of the symptoms are a result of the body shutting down. The patient will probably be bedridden, and uncommunicative. Other common symptoms can include
- Difficulties communicating
- Weight loss
- Seizures
- Skin infections
- Difficulty swallowing
- Groaning, moaning, and grunting
- Increased sleeping
- Incontinence
- Loss of mobility (if not bedridden)
- Puzzling behavior, including agitation late into the day known as “sundowning”, aggressive reactions, rocking back and forth or repeating words as soothing mechanisms, hallucinations, restlessness, and excessive hand activity
Late-stage dementia sufferers may experience a range in symptoms and symptom severity, especially as the person continues to deteriorate. The Alzheimer’s Society offers tips on how to help minimize discomfort and distress for someone suffering these symptoms.
Caretaking
In a recent study, researchers found end-stage dementia patients were being ‘slammed around the healthcare system‘ by being transferred back and forth between hospitals and nursing homes in the last days of their lives. This treatment is detrimental to the health of the patient, not only causing more distress and confusion, but also increasing the number of serious health complications. For example, patients with dementia transferred from nursing homes to hospitals were two times more likely to be in an intensive care unit in the last month of their life and three times more likely to have a bedsore.
Based on these findings and additional research, experts are now advocating end-stage dementia patients be treated with an approach similar to terminally ill cancer patients. Using a palliative care, or a pain-management approach to care, in which caregivers and doctors aim to keep the patient as comfortable as possible during the end of their life, end-stage dementia patients retain a higher quality of life. More aggressive treatment, like restraining patients to place feeding tubes, or transferring them to hospitals, does not seem to either extend their lives or improve the quality of them.
Introducing The Approach
Researchers are actively examining how to introduce a palliative care approach to more end-stage dementia patients, family members, and medical professionals. Some advocate more education and awareness around palliative care approaches and what that looks like specifically for individual families. Others suggest there are simply not enough medical providers educated in palliative care approaches and this inability to meet the demand for care remains as a strong barrier for patients receiving appropriate care.
The end-stage of dementia is tough on everyone involved in the love and care of the person suffering from the disease. Experts also acknowledge family members must care for themselves during this incredibly demanding time in their lives, as they, too, must acknowledge the beginning of the end of their loved one’s life. Alzheimer’s Stages – Early, Middle, Late Dementia Symptoms | alz.org
Learn More:
End Stage Of Dementia
Alzheimer’s doesn’t have to be your brain’s destiny, says neuroscientist and author of “Still Alice,” Lisa Genova. She shares the latest science investigating the disease — and some promising research on what each of us can do to build an Alzheimer’s-resistant brain.
Cliff notes version – He is saying that he took Razadyne, Curry, Omega 3 Fish Oil with high amounts of DHA, organic flax seed meal on cereal, Vitamin D3, Vitamin B12 (Chicken livers, heart and gizzards to augment B12 Vitamin – eaten 2-3 times a week), Multivitamin with no iron. Take the Razadyne and vitamin supplements every day regularly or you will regress. It takes several months for this cocktail to work.

One Response to Alzheimer’s Disease