© Provided by Discover Magazine
When I was 9 years old, I had a Deep Fascination with,
“That’s one small step for man, one giant leap for mankind.”
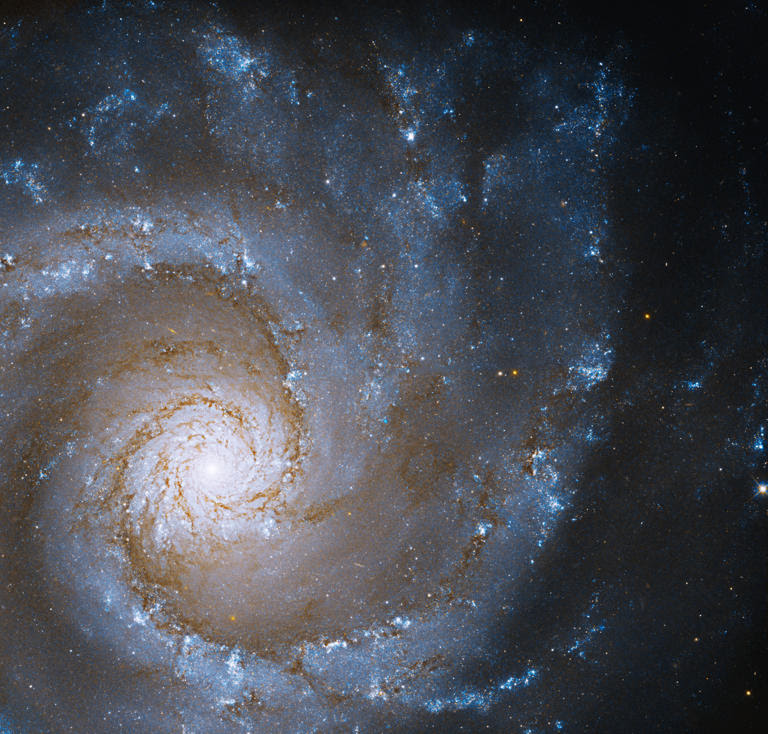
Our universe is about 13.8 billion years old, and the observable bubble of that cosmos has a diameter of about 93 billion light-years across. And we all know the famous maxim from Albert Einstein’s special theory of relativity: nothing can travel faster than light.
Taken together, this presents us with a perplexing riddle about the nature of the cosmos itself: How can the universe get so mind-bogglingly big in such a short amount of time?
What Does “Faster Than Light” Mean?
There are two ways to answer this question. The two ways are perfectly equivalent mathematically, but one or the other might make more sense to you.
Einstein’s Special Theory of Relativity
The first way is to point out that Einstein’s special theory of relativity is a local theory of physics. It tells you that if a rocket were to blast off in front of your face, you will never, ever record its speed as going faster than light.
The very concept of “speed” is only something that you can measure nearby your current position. Special relativity is absolutely silent about the behavior of objects on the far side of the universe – concepts like the speed of light limit simply don’t apply to them, because they’re too far away and special relativity no longer applies.
Einstein’s Theory of General Relativity
To grapple with distant objects, you have to employ a broader, more general theory, like Einstein’s theory of general relativity, which describes how gravity influences the fabric of space-time.
In other words, the most distant galaxies can apparently go faster than the speed of light because, essentially, the universe doesn’t have to care about the speed of light.
Read More: Will Humans Ever Go Faster Than Light?
An Expanding Universe
And it’s in general relativity that we get our second way to solve the riddle.
According to this model, which is how we currently understand the cosmos,
we live in an expanding universe. Every day, our cosmos gets bigger and bigger,
with the average distance between galaxies always getting larger.
So far, so good, right? But that expansion isn’t caused by galaxies moving in the universe, but rather the space between the galaxies expanding.
If you were to attach an accelerometer to every galaxy, they would register zero movements (except for small, local motions here and there.)
Locally, no galaxy is moving. But the space between them is. So there are no restrictions here based on the speed of light because they’re literally not moving. There’s no limit to how quickly space can expand (because “expanding” isn’t a motion as far as relativity is concerned) and so the universe can grow as quickly as it pleases.
Related video: Watch This Amazing James Webb 4K Space Telescope View Of The Cosmic Cliffs (Dailymotion)
Is the Observable Universe?
Essentially, the universe is so big because it can expand faster than light. In fact, it’s doing so today. We measure the present-day expansion rate of the universe with something called the Hubble constant, which is around 68 kilometers per second per megaparsec.
That means for every megaparsec in distance you get away from the Milky Way, the universe’s expansion speed will increase by 68 km/s. A galaxy two megaparsecs away appears to recede at 136 km/s, a galaxy ten megaparsecs away will recede at 680 km/s, and so on.
Read More: How Did the Universe Begin?
The Hubble constant guarantees that once you reach a certain distance — about 13 billion light-years (a distance known as the Hubble radius) — galaxies will appear to move away from us faster than light. The same would be true if you and I were to stand on opposite ends of a stretchy rubber band.
As long as the rubber band didn’t break, as long as the stretching maintained a constant speed, at some point we would appear to be moving away from each other faster than light. (And yet, once again to emphasize this point, if we were to draw an “X” at our feet, we wouldn’t have moved away from those spots).
Distant Galaxies
The light from galaxies beyond the Hubble radius was released billions of years ago and is only just now reaching the Earth. We calculate where these galaxies are right now based on our understanding of cosmology, and that’s how we’re able to estimate the size of the universe. The fact that they appeared to move faster than light means that any light that they send now will never reach us — because that light will not be able to overcome the expansion of the universe.
Since most of the universe is beyond the Hubble radius, all those galaxies are forever out of reach. As time goes on, those galaxies will, one by one, disappear entirely from view. Not through any cheating of the laws of physics, but through simple (and inevitable) stretching.
Read More: NASA says the solar eclipse cutting from Texas to Maine in April will be way cooler than any before it. Here’s why. (msn.com)
The Universe May Be a Hologram, Meaning Our Entire Reality Could Be an Illusion.
Scientists discover secret symmetries the protect earth from the chaos of space.
Black Holes Are Accelerating the Expansion of The Universe, Say Cosmologists

This age-old question has been dubbed Olbers’ paradox. © John Moore via Getty Images.
What is Olbers’ Paradox? – Search (bing.com)
Why is space so dark even though the universe is filled with stars?
Story by Brian Jackson, Associate Professor of Astronomy, Boise State University
Curious Kids is a series for children of all ages.
If you have a question, you’d like an expert to answer, send it to curiouskidsus@theconversation.com.
Why is space so dark despite all of the stars in the universe? – Nikhil, age 15, New Delhi
People have been asking why space is dark despite being filled with stars for so long that this question has a special name – Olbers’ paradox.
Astronomers estimate that there are about 200 billion trillion stars in the observable universe. And many of those stars are as bright or even brighter than our sun.
So, why isn’t space filled with dazzling light?
I am an astronomer who studies stars and planets – including those outside our solar system – and their motion in space. The study of distant stars and planets helps astronomers like me understand why space is so dark.
You might guess it’s because a lot of the stars in the universe are very far away from Earth. Of course, it is true that the farther away a star is, the less bright it looks – a star 10 times farther away looks 100 times dimmer. But it turns out this isn’t the whole answer.
Imagine a bubble
Pretend, for a moment, that the universe is so old that the light from even the farthest stars has had time to reach Earth. In this imaginary scenario, all of the stars in the universe are not moving at all.
Picture a large bubble with Earth at the center. If the bubble were about 10 light years across, it would contain about a dozen stars. Of course, several light years away, many of those stars would look pretty dim from Earth.
If you keep enlarging the bubble to 1,000 light years across, then to 1 million light years, and then 1 billion light years, the farthest stars in the bubble will look even more faint. But there would also be more and more stars inside the bigger and bigger bubble, all of them contributing light. Even though the farthest stars look dimmer and dimmer, there would be a lot more of them, and the whole night sky should look very bright.
It seems I’m back where I started, but I’m actually a little closer to the answer.
Age matters
In the imaginary bubble illustration, I asked you to imagine that the stars are not moving and that the universe is very old. But the universe is only about 13 billion years old.

Galaxies as they appeared approximately 13.1 billion years ago, taken by the James Webb Space Telescope. © NASA/ESA/CSA/STScI/Handout from Xinhua News Agency.
Even though that’s an amazingly long time in human terms, it’s short in astronomical terms. It’s short enough that the light from stars more distant than about 13 billion light years hasn’t actually reached Earth yet. And so the actual bubble around Earth that contains all the stars we can see only extends out to about 13 billion light years from Earth.
There just are not enough stars in the bubble to fill every line of sight.
Of course, if you look in some directions in the sky, you can see stars. If you look at other bits of the sky, you can’t see any stars. And that’s because, in those dark spots, the stars that could block your line of sight are so far away their light hasn’t reached Earth yet.
As time passes, light from these more and more distant stars will have time to reach us.
The Doppler shift
You might ask whether the night sky will eventually light up completely. But that brings me back to the other thing I told you to imagine that all of the stars are not moving.
The universe is actually expanding, with the most distant galaxies moving away from Earth at nearly the speed of light.
Because the galaxies are moving away so fast, the light from their stars is pushed into colors the human eye can’t see. This effect is called the Doppler shift. So, even if it had enough time to reach you, you still couldn’t see the light from the most distant stars with your eyes. And the night sky would not be completely lit up.
If you wait even longer, eventually the stars will all burn out – stars like the sun last only about 10 billion years. Astronomers hypothesize that in the distant future – a thousand trillion years from now – the universe will go dark, inhabited by only stellar remnants
like white dwarfs and black holes.
Even though our night sky isn’t completely filled with stars, we live in a very special time in the universe’s life, when we’re lucky enough to enjoy a rich and complex night sky, filled with light and dark.
Hello, curious kids! Do you have a question you’d like an expert to answer?
Ask an adult to send your question to CuriousKidsUS@theconversation.com.
Please tell us your name, age and the city where you live.
And since curiosity has no age limit – adults, let us know what you’re wondering, too. We won’t be able to answer every question, but we will do our best.
This article is republished from The Conversation, a nonprofit news site dedicated to sharing ideas from academic experts.
Read more:
Why is astronomy a science but astrology is not?
Why does the Moon look close some nights and far away on other nights?
With all eyes on Portland’s fentanyl crisis, many rural Oregon communities dealing
with their own opioid and homelessness epidemics feel abandoned by policy makers.
Crisis in the Northwest: The homeschool mom documenting Portland’s ‘destruction’.
Crisis in the Northwest: Rural Oregon struggles to contain fentanyl epidemic.
Why traveling to witness a total solar eclipse is so worth it (msn.com)
How do astronomers know the age of the planets and stars? (msn.com)
2024 Solar Eclipse: The 13 Best Cities to See the Phenomenon (msn.com)
The Real Problem with American Culture (msn.com)
How We Find Our Place in the Universe (msn.com)
Where is the center of the universe? (msn.com)
Is the vacuum of space truly empty? (msn.com)
Is the Universe Expanding? (msn.com)
How far apart are stars? (msn.com)
Brian Jackson receives federally funded research grants from NASA.
The science behind the Big Bang theory (msn.com)
The first suggestion of the Big Bang was in 1912.
Later in the 1930s, Edwin Hubble used the world’s largest telescope and showed that the distant galaxies all appeared to be receding from us. That means that the farther away they are, the faster they are retracting. The first and most confident evidence we have came from 1964 when scientists at the Bell Labs discovered the cosmic microwave background radiation, confirming there was a Big Bang. This revolutionized cosmology, how we see the universe, and how we view our place within it. Scientists have come up with several possible explanations for what happened before the Big Bang, if anything at all, and it is entirely possible that there was no previous era. Assuming this is true, it means that matter, energy, space, and time just began abruptly.
What happened after the Big Bang?
What happened immediately after the explosions is called the Planck Era: the earliest known period of time. According to the theories of physics, one second after the Big Bang, the heat of the universe caused atoms to collide with enough force to create a ten billion degree soup of neutrons, protons, electrons, positrons, photons, and neutrinos. Essentially, cosmic inflations created a soup of sub atomic particle plasma. It appears that this is what gave rise to dark matter and likely the phase in which matter gains superiority over antimatter.
Within the first 300 seconds of the existence of the universe, the elements hydrogen, helium, and some lithium form from the protons and neutrons. This process is called nucleosynthesis and is a theory that accurately predicts the abundances of elements and isotopes found in the early samples of the universe, like some of the oldest stars.
This verification is a strong indication that our model of the universe is accurate.
300,000 years later, when the nearly uniform soup cooled, atoms formed other nuclei.
Photons ceased to scatter through space, turning the prior opaque universe into one with visible light. Those same photons, the actual afterglow of the Big Bang known as cosmic background radiation, can still be observed today.
The cosmic background radiation and the Big Bang
Space agencies have launched three missions to study this cosmic background radiation, taking baby pictures of the universe only 400,000 years after its birth. The first two probes map the primordial hot and cold spots in cosmic background radiation, measuring temperature differences that are nearly uniformly distributed across the universe. A third mission, with instruments sensitive to temperature variations of a few millions of a degree, made the most accurate maps of the microwave background radiation yet.
The dark ages before stars were born
About one million years after the Big Bang, we enter a period called the Dark Ages, which is known as the final frontier of cosmology. Little is known about this period, except that it was the period before the first stars were born. The Dark Ages are thought to have lasted about 100 million years. However, due to the limit of current observations, the oldest objects we can see are at a time when the universe was only several hundred million years old. Two future projects that have already begun construction, are specifically designed to shed some light on this era and hopefully bring the Dark Ages to an end.
Then, ten billion years after the Big Bang, dark energy, a mysterious force starts to accelerate. After that, 13.8 billion years after the Big Bang, we reach our time today.
The end of the universe
The ultimate fate of the universe all hinges on dark energy. If the universe continues to grow at about the same pace, 30 billion years from now, all the galaxies would be pulled from our view and all the evidence of the Big Bang would be completely lost forever. This would result in all the last stars burning out in about 100 trillion years, so we have plenty of time left.
Dark energy could also intensify resulting in a Big Rip scenario. This would happen in approximately 50 billion years from now. Dark energy would effectively tear everything apart, from superclusters to atoms. On the contrary, if dark energy slowed down,
then this would give gravity the upper hand and lead to a collapse 30 billion years
from now, ultimately resulting in a Big Crunch.
Related video: Top 10 Questions We Have About The Big Bang Theory After Watching Young Sheldon (Dailymotion) – Search (bing.com)
The post The science behind the Big Bang theory appeared first on Astronomy Magazine
The Earth is a sphere with four seasons because the Earth is tilted at an angle if the Earth was not a sphere and was flat no life would be able to exist. I cannot believe human beings are capable of believing in a flat Earth. It’s impossible but you have the right to believe the way you want to. Earth may have had all the elements needed for life within it all along − contrary to theories that these elements came from meteorites (msn.com)
On A Cosmic Scale, The Universe Is Quite Small — This Could Transform Our Understanding Of It (msn.com)
7 discoveries that prove Einstein was right about the universe — and 1 that proves him wrong (msn.com)
‘You Can Learn Lessons From the Darkness’: What It’s Like to Have Cancer at a Young Age (msn.com)
Biden calls for broad new social programs, higher taxes on corporations and the wealthy.
Joe: The contrasts couldn’t be greater between Biden, Trump in dueling rallies | Watch.
Has Biden done anything that’s actually good for America?: Sen. Josh Hawley | Watch.
How a ‘hum’ from space helped scientists show the universe is in constant movement.
I regret moving to Florida. Living here felt like paradise — until everything changed.
The Universe May Be a Hologram, Meaning Our Entire Reality Could Be an Illusion.
Study: “Woke” attitudes linked to anxiety, depression, and a lack of happiness (msn.com)
Missing ‘Law of Nature’ Found That Describes The Way All Things Evolve (msn.com)
The Bizarrely Unbalanced Early Universe Might Explain Why We Exist (msn.com)
China’s underground neutrino lab unveils the mysteries of the universe (msn.com)
Life’s building blocks may have formed near newborn stars and planets (msn.com)
The total amount of life that has ever existed on Earth is mind-blowing (msn.com)
How did life on Earth begin? The chemical puzzle just became clearer. (msn.com)
Tulsi Gabbard Warns of Major Challenges for Biden-Harris Campaign (msn.com)
What scientists learned after strapping a collar camera to polar bears (msn.com)
Comet that passes Earth once every 71 years now visible in night sky (msn.com)
Study gives new insight into how life on Earth may have started (msn.com)
Scientists propose a “missing law” for evolution in the universe (msn.com)
Scientists unveil ‘missing’ law of nature in landmark discovery (msn.com)
“God Doesn’t Exist” America’s Most Atheist States (RANKED) (msn.com)
Three billion people will live in uninhabitable zones by 2070 (msn.com)
Trump vs. Biden: Who Is Leading in Every Swing State (msn.com)
‘It is all but impossible life exists, and yet it is here’ (msn.com)
The Universe Is Nothing Without Us (msn.com)
Easter reminds us that life is fundamentally good,
not some kind of divine blunder.




 𝐍𝐢𝐧𝐞𝐯𝐞𝐡, 𝐓𝐞𝐱𝐚𝐬
𝐍𝐢𝐧𝐞𝐯𝐞𝐡, 𝐓𝐞𝐱𝐚𝐬