As a doctor, here’s what I have learned from my own Alzheimer’s disease
Story by Daniel Gibbs – Search Videos
I have a special interest in Alzheimer’s disease. For nearly 25 years, I practiced general neurology in Portland, Oregon, and some of my patients had dementia. In 2012, while doing a genealogical DNA search, I inadvertently discovered that I have two copies of the APOE-4 allele, meaning I had a very good chance of getting Alzheimer’s-caused dementia by age 80.
I felt Gobsmacked.
I remember walking down the stairs in a daze after reading the report from the genetic testing service and telling my wife, Lois, “I think I am screwed.”
A year later, I retired at age 62 even though I had no symptoms of cognitive impairment. If I had almost any other job, I could have continued working for a few more years, but in medicine, forgetfulness could have fatal consequences. I suddenly wore two hats — that of a retired physician who had cared for a lot of people with Alzheimer’s disease and now a person living with the same disorder.
I had been taught, in medical school in the 1970s and even during my neurology residency in the 1980s, that Alzheimer’s disease progresses from onset to death in about three to five years, and nothing can be done about it. Neither statement is true.
In hindsight, my first symptom of Alzheimer’s disease was a gradual loss of smell that I first noticed in 2006. This was accompanied by odd olfactory hallucinations that smelled like baking bread mixed with perfume. I didn’t have any measurable cognitive impairment until 2015, when I had significant trouble remembering words, including the names of friends and colleagues.
 Related video: What Is Alzheimer’s Disease? (Newsweek) – Search
Related video: What Is Alzheimer’s Disease? (Newsweek) – Search
I had a PET scan as part of a research study, which showed my brain had the beginning of abnormal tau protein, a key part of diagnosing Alzheimer’s. When the scans were repeated in 2018 and 2022, the tau protein can be seen spreading through my brain.
We now know that the first signs of Alzheimer’s disease, beta-amyloid plaques, can be seen in the brain up to 20 years before any cognitive changes. Tau-containing tangles start to form later, about two or three years before the onset of mild cognitive impairment. There is a variation in the speed of progression from mild impairment to full-blown dementia to death, probably about eight to 12 years on average.
I am now 73, and I have had mild cognitive impairment for roughly five years, followed by mild dementia for about four years. We don’t yet have a way to stop this progression, but what have I been doing to slow it?
There are lifestyle modifications that help, and they also decrease the likelihood of getting it in the first place.
Top among them is aerobic exercise.
Multiple studies have shown up to a 50 percent reduction in the chance of getting Alzheimer’s disease for people who exercise regularly. The only group that doesn’t seem to benefit from exercise are those who already have dementia. The sooner you start, the better.
I started exercising daily in 2012 as soon as I learned that I was on the Alzheimer’s trajectory. Recent evidence shows that tai chi can help people who already are experiencing cognitive impairment.
The data for adopting a plant-based diet are almost as strong as exercise. I follow a variant of the Mediterranean diet called the MIND diet that includes eating foods with increased flavonols such as nuts and certain vegetables. Many experts now recommend avoiding alcohol, especially for people with a family history of dementia. Recently, I gave up my daily glass of beer or wine. Frankly, I have been surprised that nonalcoholic beer tastes quite good.
Staying mentally active is very important. For me, my most important brain exercise is reading and writing. I do a crossword puzzle every day while eating lunch, and I enhance the brain benefit by looking up words I don’t know. Staying socially engaged is important but increasingly difficult as dementia progresses. It’s best for me to socialize with just one or two people at a time. Getting at least 7½ hours of sleep each night appears to reduce the chance of getting dementia.
What about drugs?
We now have two FDA-approved drugs, lecanemab and donanemab, that are effective in removing beta-amyloid from the brain, but they only slow cognitive decline by about 35 percent. They can also have lethal side effects in patients with two copies of the APOE-4 allele, like me. After only four monthly injections of aducanumab (a cousin of lecanemab) during the phase 3 trial, I developed swelling and bleeding in my brain requiring a stay in an intensive care unit and about four months to recover. The drug has since been discontinued by its manufacturer.
These treatments represent an important step forward in understanding the neurobiology of Alzheimer’s disease, but they should not be used by everyone. So I have learned that Alzheimer’s disease is not the rapidly progressive dementia I was taught about in medical school. It is a slowly progressive disease that is asymptomatic for up to 20 years. Mild symptoms of cognitive impairment may be annoying but usually can allow normal activities for another five years or so.
Even work may be possible with accommodations. Once someone has dementia, unable to live independently, lifestyle modifications and medications do not seem to be as effective. In my experience, it is critical to manage Alzheimer’s disease in the early stages to postpone the onset of dementia. Don’t wait for the horses to get out of the barn.
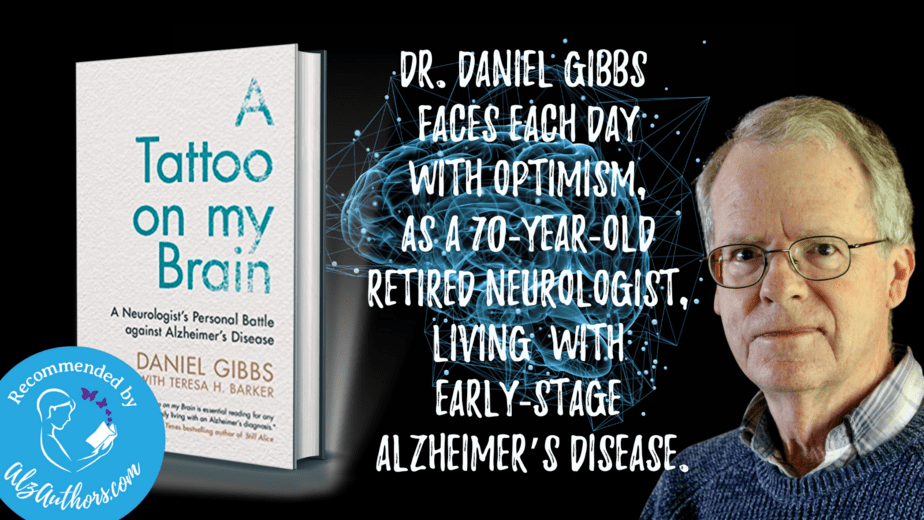
Daniel Gibbs has published two books about his experiences with Alzheimer’s disease, “Dispatches From the Land of Alzheimer’s” and “A Tattoo on My Brain: A Neurologist’s Personal Battle against Alzheimer’s Disease,” which was made into a documentary film that can be streamed on Paramount Plus. Gibbs also has a blog.
About the book – A Tattoo On My Brain

FILE – A doctor checks the blood pressure of A 94-year-old woman in Sant Sadurní d’Anoia, Catalonia region, Spain, Friday, July 31, 2020.© Felipe Dana/AP Photo
How to lower your dementia risk as cases expected to rise by 2060
Research shows that dementia cases are going up, with a study released this week estimating that cases in the United States, for instance, will double by 2060.
The study, published in the journal Nature Medicine on Monday, found that the risk of developing dementia after age 55 is double that reported by previous studies, estimating it at 42 per cent. They said this was tied to population ageing.
Previous research has estimated that global cases of dementia will rise due to population ageing and growth including a 2022 study that estimated global cases could rise from 57.4 million cases in 2019 to nearly 153 million in 2050.
Western Europe would see an estimated 74 per cent increase in cases by 2050, central Europe would have an 82 percent increase, and eastern Europe would see a 92 per cent increase, according to the study.
Related
- New dementia patients can expect to live fewer than five years after diagnosis, major analysis finds
But people can take steps to reduce their risk of dementia, such as controlling high blood pressure and other bad-for-the-brain health problems, and it’s not too late to try even in middle age.
“All of our research suggests what you do in midlife really matters,” said Dr Josef Coresh, the study’s co-author from New York University (NYU) Langone Health in the US.
Dementia isn’t only Alzheimer’s
Dementia is the progressive loss of memory, language, and other cognitive functions.
Alzheimer’s is the most common form, and silent brain changes that eventually lead to it can begin two decades before symptoms appear. Other types include vascular dementia when heart disease or small strokes impair blood flow to the brain.
Many people have mixed causes, meaning vascular problems could exacerbate brewing Alzheimer’s symptoms.
Related
Measuring the risk from a certain age over the potential remaining life span can guide public health recommendations and medical research.
“It’s not a guarantee that someone will develop dementia,” said Dr James Galvin, a University of Miami Alzheimer’s specialist. He wasn’t involved with the new study but said the findings fit with other research.
Dementia risk is different by age
Prior studies estimated about 14 percent of men and 23 percent of women would develop some form of dementia during their lifetime.
Coresh’s team analysed more recent data from a US study that has tracked the heart health and cognitive function of about 15,000 older adults for several decades. Importantly, they found the risk changes with the decades.
Only 4 percent of people developed dementia between the ages of 55 and 75, what Coresh calls a key 20-year window for protecting brain health.
Related
For people who survive common health threats until 75, the dementia risk then jumps to 20 per cent by age 85 and 42 per cent between ages 85 and 95.
Overall, the lifetime dementia risk after age 55 was 35 per cent for men and 48 per cent for women, the researchers concluded.
Women generally live longer than men, a main reason for that difference, Coresh noted. Black Americans had a slightly higher risk, 44 per cent, than white people at 41 per cent.
Ways to lower dementia risk
There are some risk factors people can’t control, including age and whether you inherited a gene variant called APOE4 that raises the chances of late-in-life Alzheimer’s.
But people can try to avert or at least delay health problems that contribute to later dementia.
Coresh, for example, wears a helmet when biking because repeated or severe brain injuries from crashes or falls increase the risk of later-in-life dementia.
Especially important: “What’s good for your heart is good for your brain,” added Miami’s Galvin. He urges people to exercise, avoid obesity, and control blood pressure, diabetes and cholesterol.
Related
For example, high blood pressure can impair blood flow to the brain, a risk not just for vascular dementia but also linked to some hallmarks of Alzheimer’s.
Similarly, the high blood sugar of poorly controlled diabetes is linked to cognitive decline and damaging inflammation in the brain.
Stay socially and cognitively active, too, Galvin said. He urges people to try hearing aids if age brings hearing loss, which can spur social isolation.
“There are things that we have control over, and those things I think would be really, really important to build a better brain as we age,” he said.
Researchers discover the mechanism that links a diet rich in fats with Alzheimer’s disease
The Symptom I Chalked Up To Old Age That Turned Out To Be Early Alzheimer’s Disease
9 Things You Should Do for Your Brain Health Every Day, According to Neurologists
Nearly Half Of Americans Over 55 May Develop Dementia By 2060: Study
Dementia Risk Dropped With Anti-Inflammatory Diet for Certain Patients
Good obesity? Healthy obesity reduces Alzheimer risk, study finds
13 Things Neurologists Do to Help Prevent Alzheimer’s Disease

