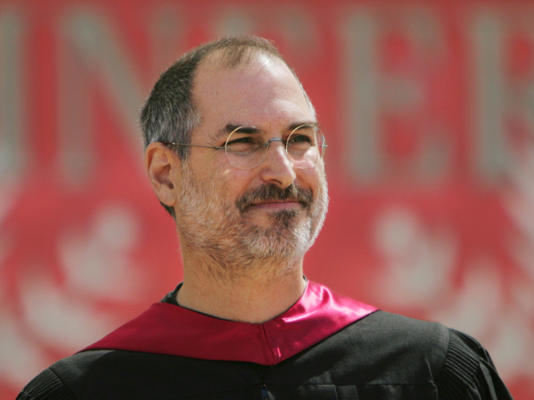
Steve Jobs spoke at the 114th commencement at Stanford University in Stanford, California on Sunday, June 12, 2005. Photo by MediaNews Group/The Mercury News via Getty Image© Provided by Business In
The Puzzle of Pancreatic Cancer:
How Steve Jobs Did Not Beat the Odds—
but Nobel Winner Ralph Steinman Did!
Despite having the same name, the diseases that killed Apple co-founder Steve Jobs and 2011 Nobel laureate Ralph Steinman are different kinds of cancer. Researchers are looking for new ways to diagnose and treat both.
By Katherine Harmon on October 7, 2011
- Apple’s Steve Jobs gave the commencement address at Stanford University on June 12, 2005.
- He told three stories about love, death, and following your gut.
- It’s been 18 years since Jobs delivered the speech, and the lessons he shared continue to resonate.
On January 9, 2007, Steve Jobs introduced the world to the iPhone.
In honor of the smart phone’s game-changing impact on personal electronics and communications, I am republishing the following story about Jobs’ battle with cancer, published shortly after his death in 2011.
Steve Jobs was a rare case, right down to his death. Announced Wednesday, Jobs’s death from “complications of pancreatic cancer” only hints at the vast complexity of the disease to which he succumbed at the age of 56.
Jobs joined recently announced Nobel Prize winner Ralph Steinman, actor Patrick Swayze and football great Gene Upshaw as the latest bold-faced name to die from this aggressive disease—one that even he, with his vast fortune, and Steinman, with his use of experimental immunological treatments, could not forestall indefinitely.
Most pancreatic cancers (53 percent) are diagnosed after they have spread—and those have an exceedingly low survival rate, with just 1.8 percent of patients living for more than five years after diagnosis. (For all types of the cancer, the average five-year survival rate when diagnosed is only slightly higher at 3.3 percent.) So how did Jobs, who was diagnosed in the fall of 2003—and who revealed it publicly in 2004—manage to survive for eight years?
Jobs had a rare form of the cancer, known as neuroendocrine cancer, which grows more slowly and is easier to treat, explains Leonard Saltz, acting chief of the gastrointestinal oncology service at Memorial Sloan-Kettering Cancer Center. “Survival for many years or even decades with endocrine cancer is not surprising.” For that type, the sort that Jobs had, “survival is measured in years, as opposed to pancreatic cancer, which is measured in months.”
“When you have a pancreatic neuroendocrine tumor, that is substantially different from pancreatic cancer,” Saltz says. Steinman, on the other hand, did have the type that is usually fatal within a year after diagnosis.
“Ralph had the garden variety, poorly differentiated pancreatic cancer,” says Sarah Schlesinger, an associate professor of immunology and cell physiology at The Rockefeller University, where she worked with Steinman.
Given the grim prognosis for both these forms of cancer, researchers are hard at work trying to develop better treatments and diagnostics, and to figure out just why one patient might live for eight years—and another for eight months.
Two different kinds
Pancreatic cancer is a rare disease, with about 44,000 new cases diagnosed in the U.S. each year, and a lifetime risk of getting it at about 1.4 percent. The vast majority of those cancers—some 95 percent—are known as adenocarcinomas, the sort that Steinman had. Jobs’s form, known as pancreatic neuroendocrine tumor (pNET), makes up the small fraction of other pancreatic cancer sufferers.
The pancreas itself is essentially two different organs, which means two distinct kinds of tissue—and two very different types of cancer, Saltz points out. The most common kind of pancreatic cancer, the adenocarcinomas, originate in what is known as the exocrine portion of the pancreas. This is the main mass of the organ, which makes digestive enzymes that get shuttled to the gastrointestinal tract via specialized ducts.
“Scattered in that larger organ are thousands of tiny islands,” Saltz explains. “These are islands of endocrine tissue,” which makes hormones that are secreted into the blood. It was a cancer of these islet cells that Jobs had.
Difficult to diagnose
Pancreatic cancer is so deadly in large part because it is often caught at a very late stage. Unlike lung or colon cancer, it does not create a lot of early symptoms. Saltz said he was hesitant to even list the manifestations (which include upper abdominal pain, weight loss, appetite loss and blood clots) because they are such common complaints that, he noted, everyone would go home and decide by this evening that they had pancreatic cancer.
Most cases are discovered after some symptoms persist or more severe indications, such as jaundice, occur.
Some groups are looking for a better way to screen for pancreatic cancer, in hopes of catching it earlier. “There’s a big push for developing a blood test,” says Philip Arlen, president and CEO of Neogenix Oncology, Inc., a company that is looking into both diagnostics and treatment for pancreatic cancer. They have found a couple of genetic markers that are present in pancreatic cancer but not in normal tissue. The goal, says Arlen, who previously worked as a researcher at the National Cancer Institute, is to develop something akin to a PSA (prostate-specific antigen) test for prostate cancer.
There are clues, for example, that pancreatic cancer is not as much a sudden-onset disease as it often seems. After studying the accumulation of genetic mutations in pancreatic cancer tumors, researchers concluded that the disease takes an average of seven years to form a substantive tumor and closer to a decade to start moving to other organs, according to research published last October. Armed with that knowledge and the other finding of pre-malignant lesions, Arlen is hopeful that a non-invasive screening method will eventually be developed.
Widespread screening for more common cancers, such as breast, colon and prostate, have come under fire lately for leading to too many false positives and excessive follow-up treatment. With even rarer diseases, it is much trickier, Saltz points out, and would demand an exceedingly low false-positive rate. “Pancreatic cancer, although it’s a terrifying disease, is rare,” he says.
Trying new treatments
When pancreatic cancer is caught early, doctors will usually try to remove it surgically. As Saltz points out, however, the chances that it will come back in the next year or two are still relatively high. And the surgery itself is risky. The pancreas is lodged deep within the abdomen, surrounded by—and connected to—other major organs. “It’s considered the magnum opus of a surgeon’s repertoire,” she says of partial pancreas removal, which is known as the Whipple procedure.
If the cancer has already spread, as it had in Steinman’s case, the most common approach is chemotherapy, which “for regular pancreatic cancer, is not very effective,” Saltz says. The mainstay is the chemo drug gemcitabine (Gemzar), which is one of the treatments Steinman received. In trials, some patients saw no benefit, but for a minority, it extended life by as long as a few years, suggesting that an essential molecular difference exists in their tumors.
Despite initial positive signs from chemo, and even when Steinman was doing better:
“He felt like he was living with Damocles’ sword over his neck—he never knew when it was going to come back,” Schlesinger says. So he turned to what he knew: the immune system. “Ralph felt deeply that the key to a cure is getting the immune system revved up enough to fight off the tumor,” Schlesinger says. “That wasn’t such a simple thing to do.”
Enlisting the immune system to fight off cancer has long been a goal of researchers.
The only immunotherapy currently approved for general use as cancer treatment is a drug for metastatic melanoma (ipilimumab, or Yervoy, approved in March). Saltz calls that approval good “evidence that it’s an important avenue to explore” for other forms of cancer.
Scientist as test subject
When word spread that Steinman had pancreatic cancer, Schlesinger says, there was an outpouring of offers from fellow immunologists to try treatments they were working on—many having been made possible by Steinman’s own discoveries about the immune system’s dendritic cells. Not all the experimental drugs were meant to tackle pancreatic tumors; some were for skin or prostate cancer.
In all, Steinman tried eight different experimental therapies, Schlesinger says. But they were not under-the-table, backroom needle jabs, she is quick to point out. Each drug was already being tested on other patients in phase I clinical trails, and Schlesinger and Steinman went through great pains—and many hours—to ensure all of the proper institutional and government approvals were granted before he got the therapies.
The first treatment he got was a vaccine called GVAX, under development to treat prostate cancer. He also received a novel therapy that worked on a developmental pathway (the hedgehog signaling pathway) and two that were based on dendritic cells: one in which dendritic cells were created from his own blood cells that were then “pulsed with RNA that had been isolated from his tumor,” Schlesinger explains; and another in which the dendritic cells were filled with “peptides that were from his own tumor.” The hope was that the RNA and proteins from his tumor would help his dendritic cells stimulate his immune system to attack the cancer.
Arlen’s group is testing, in a phase I trial, a monoclonal antibody to treat patients with the more common form of pancreatic cancer. Preliminary data show that the antibody finds its target with some 50 to 60 percent of patients with adenocarcinoma, he says. But that does not mean that it will leave them disease-free. And he hopes that a combination of the new approaches and the more standard drugs will yield even better results—a trial that they plan to start next year.
“I think it’s far too early to say they have a treatment for any of these diseases,” Saltz concludes.
Treating Jobs’s cancer
Endocrine cancer, the variety Jobs had, is treated with a different variety of chemotherapy drugs. Two new drugs for this type were just approved by the U.S. Food and Drug Administration (FDA) earlier this year. Everolimus (sold as Afinitor) works by blocking the mTOR kinase target to alter cellular signaling and was approved in May. Sunitinib (sold as Sutent) blocks a vascular endothelial growth factor. “Neither is a cure—neither is a wonder drug for the disease,” Saltz says. “Each provides some modest benefit. “
One form of treatment that is not recommended for most pancreatic cancer is a liver transplant. Media observers surmised that the transplant Jobs received in 2009 had been necessary because the cancer had spread to his liver. And although liver failure is a common cause of death for pancreatic cancer patients, because the liver is close to the pancreas and often gets invaded by the spreading cancer, getting a new one “is not an accepted standard form of treatment,” he says, citing a lack of evidence to show that it works.
Even if the new liver staved off organ failure, the immunosuppressants necessary to avoid organ rejection “can reduce the body’s ability to fight off any cancer cells that remain,” Saltz says. And factoring the many other variables of real life, it’s ultimately not possible to conclude whether the liver transplant “made him live longer, the same or shorter—we don’t know,” Saltz remarks.
Keys for a cure
Steinman, however, is a much different case. With his collection of therapies, he did manage to beat the average odds for his type of pancreatic cancer—by years. But “which thing made the difference, we will still never know,” Schlesinger says. “My personal belief is it is a combination of therapies.” Steinman, for his part, “had so much faith in dendritic cells,” Schlesinger says. “He believed that his dendritic cells played an important part.” She notes that even though they did apply and get special, individual treatment protocols for Steinman to receive each of the experimental therapies, she never doubted what they were doing; “I only felt inadequate,” she says, having a background in dendritic cells and HIV rather than cancer research.
To truly be able to hack into the inner-workings of pancreatic cancer, “there needs to be more basic science work in humans,” Schlesinger says. Saltz points to the current efforts to better grasp the molecular and genetic differences of each tumor, in hopes of finding patterns in growth rate and treatment response, which might turn into better therapeutic targets. But much of what determines why one patient might live for seven years and another for seven months seems to depend on the biology of these cancers. Which, Saltz says, “is a nice elegant way of saying that we truly don’t understand.”
Some people will tell you it was Steve Jobs Conflicted life with his daughter Lisa or his conflicted Career Life that caused his cancer. But what I know is that he battled cancer with conventional and alternative medicine and lived seven years longer than most with neuroendocrine cancer.
When Jobs was diagnosed with pancreatic cancer in 2004, he was initially told the cancer was incurable and that he had only months to live. Later that day, he said, a biopsy revealed the cancer could be treated with surgery. “I had the surgery and thankfully I’m fine now.”
But the near-death encounter gave him certainty, he said, of what he wanted to share with the graduates. “Death is the destination we all share,” Jobs said. “No one has ever escaped it. And that is as it should be, because death is very likely the single best invention of life.”
That is, it’s important to make sure you’re living true to you.
“Your time is limited, so don’t waste it living someone else’s life,” Jobs said, adding, “Don’t let the noise of others’ opinions drown out your own inner voice. And most importantly, have the courage to follow your heart and intuition.”
Steve Jobs Conflicted Life May Have Caused His Cancer – Search (bing.com)

