U.S. covid-19 deaths fall to lowest point since March 2020
By (1) Jon Kamp, (2) Talal Ansari.
The average number of daily Covid-19 deaths in the U.S. has fallen to the lowest point in more than a year, a fresh sign that vaccinations are lessening the worst effects of the pandemic. The seven-day average for newly reported deaths fell to 432 on Thursday, according to a Wall Street Journal analysis of data collected by Johns Hopkins University. The figure hasn’t been this low since late March 2020, in the early days of the pandemic, the data show.
The current average marks the lowest point for average daily deaths after any surge during the pandemic, falling below a prior low of about 520 daily deaths early last summer, the data show. It follows a sharp drop in newly reported Covid-19 cases, with the seven-day average falling below 20,000 this week for the first time since last March. On Thursday, the average was 15,030.
“This milestone reinforces that the U.S. is in the homestretch of the epidemic, thanks to vaccinations,” said Andrew Brouwer, an assistant research scientist in epidemiology at the University of Michigan. More than half of the U.S. adult population has reached full-vaccination status, according to the Centers for Disease Control and Prevention.
For those 65 and older, that figure stands at 75%.
The high rates of vaccinations among elderly people, who are most likely to
die from Covid-19 infections, have helped push the number of deaths lower. And the steady decline in newly reported cases indicates that deaths, a lagging indicator, will continue to shrink. “Vaccinations are extremely effective against severe Covid disease and death and are now widely available,” Dr. Brouwer said.
Hospitalizations have also been consistently falling, with the latest data posted by the Department of Health and Human Services showing 23,240 Covid-19 patients in hospitals across the U.S., down from 39,810 a month ago and a high of 142,273 in mid-January. Doctors say treatment protocols for Covid-19 patients have steadily improved, and may be saving lives. But the starkest benefit is likely the vaccine.
Four out of every five Covid-19 deaths have been in people over 65,
and that population is now significantly shielded by inoculations. For people who aren’t vaccinated and get infected, drug treatments called monoclonal antibodies have helped patients recover faster and prevented them from developing severe cases, doctors say. In clinical trials, the drugs reduced the risk of hospitalization or death by 70% in people with mild-to-moderate symptoms.
The actual count of recent deaths may actually be lower. There have been several incidents of states catching up with backlogs in reporting, which have inflated recent death counts. States sometimes don’t backdate these deaths to when they occurred. Kentucky on June 1 said there were 260 previously unreported deaths found during an audit. Maryland and Oklahoma have also recently posted revisions.
These recent backlogged mortality reports have made it difficult to measure
the portion of cases that become deaths, which is another way to track how vaccines are turning the tide. Still, this ratio—which the Journal measures with a 28-day gap between cases and death to cover what experts say is a likely reporting gap between the two metrics—had recently trended lower.
Covid-19 shots are also bearing fruit in other countries that are deep into their mass-vaccination campaigns. In the U.K., where half of adults are fully vaccinated and another quarter are awaiting their second dose, daily deaths have fallen to levels not seen since early March 2020, when the pandemic was just taking hold. The seven-day average of new Covid-19 deaths in the U.K. was 7.7 Thursday, according to government data, which compares with a peak of more than 1,200 daily deaths reported during the country’s most recent wave of infection in January.
Public-health officials estimate vaccines have averted 13,000 deaths this year so far and prevented more than 39,000 hospitalizations. Despite the good news in the U.S., there are regional variations in Covid-19 metrics that could affect the pandemic in coming months. Although 52% of American adults are fully vaccinated, the percentage varies by state. At the top of the list is Vermont, where nearly 57% of the entire population is fully vaccinated.
At the bottom is Mississippi, where 27.5% of the population has been inoculated.
Last summer saw new Covid-19 cases surge across parts of the South and Southwest amid re-openings and rising temperatures that pushed more people to the air-conditioned indoors. Some epidemiologists and public-health officials worry that lower vaccination rates in the South could lead to a rise in infections this summer, though few expect case counts to reach as high as last year, given the broader vaccine uptake nationally.
Covid-19 also continues to rage in less-vaccinated parts of the world, indicating that, globally, the pandemic is far from over. High infection rates world-wide also create a continuing risk of new and dangerous Covid-19 variants, epidemiologists say. Scientists and public-health officials in the U.K. are concerned about the rapid spread there of a variant first detected in India and given the name Delta by the World Health Organization.
British data suggest that two doses of vaccine provide substantial protection against the variant but that people awaiting their second shot may be less well protected against infection. Studies have suggested that vaccines available in the U.S. protect against variants of the coronavirus that have emerged, although perhaps not as strongly as against early strains. Health officials and vaccine makers are exploring ways to prolong immunity and better protect people.
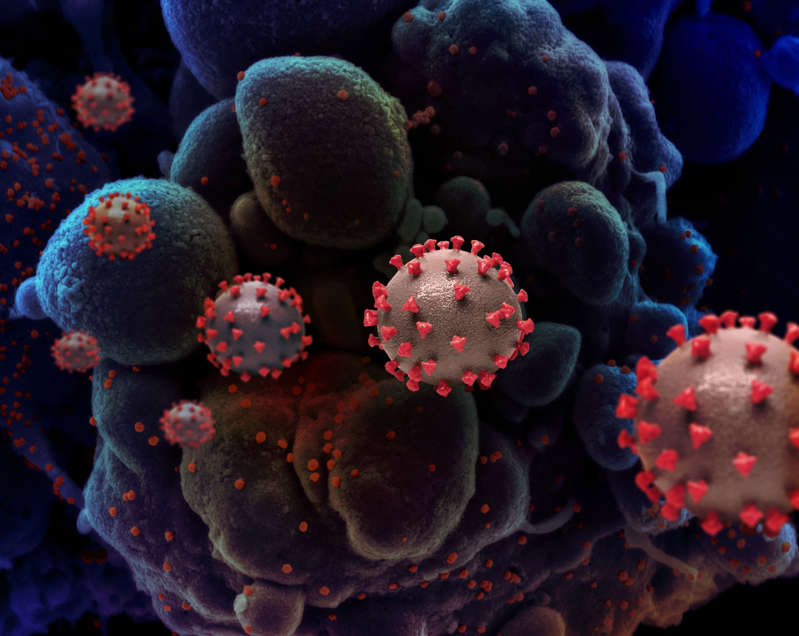
The search continues for the origins of the virus that causes COVID-19—
and the pathway it took to leap from animals to humans. Wreaking havoc across the globe, infecting more than 171 million people and killing more than 3.6 million, as of June 3. On May 26, the Biden administration directed U.S. intelligence officials to take a closer look at the virus’s origins, including zoonotic transmission—the virus spilling over from another animal to humans—and the possibility of an accidental leak from a laboratory where a wild sample containing SARS-CoV-2 might have been studied.
Until now, the biggest look into the origins of the SARS-CoV-2 virus was a World Health Organization report released on March 30 by a team of international researchers who traveled to China to investigate four possible scenarios in which the SARS-CoV-2 virus might have caused the initial outbreak. In the weeks since, however, world governments have expressed concern that the investigators lacked access to complete data, while scientists say that the report has shed little light on how the virus got jump-started.
Quick and definitive answers are impossible, given that it typically takes
years to trace a virus back to its roots—if researchers manage to do so at all, says Angela Rasmussen, a virologist at the Center for Global Health Science and Security at Georgetown University Medical Center. But in this case, she says, “I think we do have enough evidence to say that some are more likely
than others.”
In the WHO report, the team found that the virus most likely jumped from
one animal to another before making its way to humans. They also looked at evidence supporting theories that the virus passed into humans directly from an original host animal, or that it traveled through the supply chain for frozen and refrigerated foods. In addition, the team addressed the possibility that the virus had been collected in the wild and then accidentally leaked from a laboratory in Wuhan—a scenario they determined is “extremely unlikely.”
The WHO report underscores the virus’s likely natural origins, drawing on compelling evidence that SARS-CoV-2 arose in the wild and was not “engineered.” Many scientists, including Anthony Fauci, director of the U.S. National Institute of Allergy and Infectious Diseases, have long dismissed the notion that the virus was manufactured.
(See Fauci’s exclusive interview with National Geographic in which he explained why he thinks SARS-CoV-2 had a natural origin.)
Here’s a look at the evidence the WHO report lays out for each of the four theories—and what experts make of them as possible origin stories for SARS-CoV-2, the virus that causes COVID-19.
1. Direct spillover from animals to humans
WHO ASSESSMENT: possible to likely
The first origin story for SARS-CoV-2 is simple: It suggests that the virus started out in an animal—probably a bat—that came into contact with a human. Boom, infected. At that point, the virus immediately began to spread to other humans.
The WHO report cites strong evidence showing that most coronaviruses that infect humans come from animals, including the virus that caused the SARS epidemic in 2003. Bats are thought to be the most likely culprits, as they host
a virus that is genetically related to SARS-CoV-2.
The report acknowledges the possibility that the virus spread to humans from pangolins or minks. But David Robertson, head of viral genomics and bioinformatics at the University of Glasgow, says the WHO joint team sampled many animal species beyond bats for the report. The analyses point to bats as the reservoir species.
“So what you have to worry about then is how did it get from bats to humans?” Robertson says. “Did somebody go into an area, get infected, and then get a train to Wuhan?”
Direct transmission between bats and humans is possible: Studies have shown that people who live near bat caves in southern China’s Yunnan Province have antibodies to bat coronaviruses. But most humans generally don’t spend much time around bats, unless they are bat scientists (who typically wear protective equipment). So it’s unclear why, if the virus jumped from bats directly to humans, the first outbreak would have occurred in Wuhan, a thousand miles away from the bat caves of Yunnan.
Furthermore, the report notes that it would take decades for even the closely related bat coronavirus to evolve into SARS-CoV-2. Since scientists haven’t found a bat virus that would provide the missing link, the WHO team assessed this theory as “possible to likely.”
2. Spillover from animals to humans through an intermediate host
WHO ASSESSMENT: likely to very likely
In the absence of a smoking gun showing that bats passed the virus directly to humans, scientists believe the more likely theory is that the virus first traveled through another animal, such as a mink or a pangolin. Unlike bats, these animals have regular contact with humans—particularly if they’re being raised on a farm or trafficked in the illegal wildlife trade.
If the virus jumped first to another animal, that might also explain how it adapted to be harmful to humans—although Robertson says that the virus likely wouldn’t have had to change much. Genomic analyses suggest that SARS-CoV-2 is a generalist virus rather than one specifically adapted to humans, explaining why it can easily jump among pangolins, mink, cats, and other species.
The WHO report points out that this is the path that previous coronaviruses have taken to infect humans. The SARS virus, for example, is thought to have passed from bats to palm civets before causing a human epidemic in 2002. Meanwhile, the virus that causes MERS has been found in dromedary camels throughout the Middle East.
Daniel Lucey, an adjunct professor of infectious diseases at Georgetown University Medical Center, says that the similarities between SARS-CoV-2
and its relatives SARS and MERS is a compelling argument that it might
have started out the same way.
“Now we have three coronaviruses that cause pneumonia and systemic illness and death,” he says. “Past is prologue.”
But, if the theory holds true, it’s not clear what that intermediary animal might have been for SARS-CoV-2. The WHO team analyzed samples from thousands of farmed animals across China, all of which tested negative for the virus. Lucey argues that the WHO team didn’t adequately test China’s farmed mink—one of the suspected intermediaries—but Rasmussen says the report itself acknowledges that it only scratches the surface.
“That’s a fraction of the animals that are farmed or captured or transported for this purpose in China,” she says. “I think we haven’t done anywhere near enough sampling.”
3. Introduction through refrigerated or frozen foods
WHO ASSESSMENT: possible
Another theory holds that the virus may have come to humans through
what’s known as the cold chain—the supply line for distributing frozen and refrigerated foods. In this scenario, the virus might have actually originated outside of China but was imported either on the surface of food packaging or
in the food itself.
This theory gained traction last summer after a couple of outbreaks in China, and there has since been some evidence suggesting that pathogens can survive longer in cold temperatures.
Still, while the cold chain might have played a role in new outbreaks, scientists say there’s little reason to believe that it was the source of the pandemic. There’s no direct evidence that SARS-CoV-2 is responsible for foodborne outbreaks, while Rasmussen notes that COVID-19 rarely spreads through surfaces—which was good news for those weary of wiping down their groceries.
“It’s not impossible,” she says. “You can’t rule it out. But I don’t think the evidence base is particularly strong for that.”
Rasmussen says a more plausible way that the virus might spread through the food chain would be through wildlife that’s farmed for human consumption. But, she points out, that bleeds over into the territory of the theory for an intermediate host.
Some critics claim that this theory is a red herring to push suspicion from China and onto other countries. Lucey considers this pathway the least likely
of the four the joint team identified, arguing it’s implausible that the virus would have stayed viable on the packaging for as long as it took to import from Europe or elsewhere. He also questions why these infections would have turned up in Wuhan and nowhere else.
“To me, it’s beyond far-fetched,” he says.
4. Laboratory leak
WHO ASSESSMENT: extremely unlikely
The most controversial hypothesis for the origin of SARS-CoV-2 is that
the virus leaked out of a laboratory in Wuhan where researchers study bat coronaviruses. Scientists point out that for now, the evidence both for and against the accidental lab leak hypothesis is thin, but past coronavirus epidemics such as SARS and MERS occurred naturally via zoonotic transmission.
There are two versions of the lab-leak idea: that a researcher was accidentally infected in the lab, or that researchers intentionally manipulated a coronavirus strain to create SARS-CoV-2. Researchers have roundly debunked the latter idea—that SARS-CoV-2 was manufactured—since genetic evidence shows that the virus arose naturally. The WHO focused on the possibility that the virus accidentally escaped from a lab in which wild samples were being studied.
Researchers at the Wuhan Institute of Virology have sequenced the bat coronavirus strain—called CoV RaTG13, which is 96.2 percent similar to SARS-CoV-2, and its closest known relative—as part of their effort to prevent zoonotic viruses from spilling over to humans. A separate laboratory run by the Wuhan Center for Disease Control and Prevention has also worked with bat coronaviruses.
Although there have been laboratory leaks in the past, the WHO report points out that they’re rare. According to the WHO report, there is no record that any Wuhan laboratory was working with a virus more closely related to SARS-CoV-2 before the first cases of COVID-19 were diagnosed in December 2019, nor did any laboratory staff report any COVID-like symptoms suggesting that they had been infected.
On May 23, the Wall Street Journal reported that the U.S. had raw intelligence saying three researchers from the Wuhan Institute of Virology had sought hospital care in November 2019, which may have informed claims made by the Trump administration’s State Department in January. However, the State Department also noted that the Wuhan researchers’ symptoms were “consistent with both COVID-19 and common seasonal illnesses.”
Speaking in April, when the WHO report was released, Lucey said he believes the theory is plausible, though less likely than zoonotic transmission, given the lack of evidence. He points out that there was no forensic investigation of the labs in Wuhan, and he questions why the WHO authorized the team to investigate the lab at all without the mandate to conduct such an investigation or team members with the subject-matter expertise to carry it out.
“There’s not really any way to prove or disprove the lab leak theory based on what’s been presented in this report,” Rasmussen agreed at the time, noting that to put the matter to rest there would need to be a forensic audit of lab records to look for the ancestral virus to SARS-COV-2. “But my opinion is that the lab leak theory, while not impossible, is less likely to be the explanation.”
Rasmussen explains that there’s no evidence that SARS-CoV-2 is the result of genetic manipulation, nor is it likely that it could have been created by accident. It’s incredibly difficult to culture a virus that’s strong enough to cause human infections from a bat sample, she says. Meanwhile, similar viruses commonly occur in nature, making that the far likelier source.
Robertson says that supporters of the lab leak theory argue that SARS-CoV-2 has traveled too quickly and efficiently through the human population to be natural in origin. But if the virus is a generalist, as genomic studies show, he says it’s not surprising that it is so effective at infecting humans.
“I think the evidence is pretty good that it didn’t have to change much to be successful in humans,” he says. Although the WHO report may not have shed much light on the origins of SARS-CoV-2, Robertson says this is just the beginning of what can sometimes be a long process. But he says there’s a public health imperative now to launch more rigorous follow-up studies. “There’s a virus somewhere out there that’s very close to SARS-CoV-2,” he says. “That seems to be the bit that’s terrifying.”
Rasmussen says that the WHO report lays out a roadmap for further studies to discover the origins of the virus. It recommends better surveillance of captive and farmed animals to determine potential reservoir or intermediate hosts, as well as more sampling among bats—both in China and beyond, as there is also evidence of related coronaviruses circulating in regions such as Southeast Asia. The report also recommends in-depth epidemiological studies of the first COVID-19 cases.
Understanding how an outbreak got started helps scientists and governments pinpoint how to strengthen protections—whether that’s more rigorous surveillance for infections in animals and the food chain, or tighter biosafety protocols in laboratories.
“There’s a popular perception that we need some kind of justice or explanation, and somebody needs to answer for this pandemic,” Rasmussen says.
“But the real reason why we need to figure out the origin is so that it can inform our efforts to prevent another pandemic like this from happening.”
A research roadmap
The U.S. is on track to meet President Biden’s goal of partly vaccinating 70%
of adults by July 4. But 30 states are unlikely to reach the national target,
and a handful may not get there before year’s end.
These 12 states have reached or surpassed 70 percent of adults: California, Maryland, New Hampshire, Pennsylvania, New Mexico, Rhode Island, New Jersey, Maine, Connecticut, Massachusetts, Hawaii, and Vermont.
The U.S. Has Failed to Persuade Americans to Get Vaccines. Here’s How It Should Course-Correct.
Fauci Ignored Physicist Claiming Two Drugs Could Help Fight Coronavirus (breitbart.com)
We will learn the true power of COVID-19 vaccines in two weeks. Here’s why (msn.com)
Everything You Need to Know About the COVID-19 Vaccine – FAQs & Facts (cosmopolitan.com)
Can People Vaccinated Against COVID-19 Still Spread The Coronavirus? (msn.com)
Slash Your Cancer Risk in Seconds, Say Cancer Experts (msn.com)
The 6 reasons Americans aren’t getting vaccinated (msn.com)
U.S. Covid-19 Deaths Fall to Lowest Point Since March 2020 (msn.com)
After everything we now know, if you are still wearing a mask,
you should move to one of those Marxist utopias you love so much.
I’m Optimistic About Life & I Love America. You deserve freedom





