
 Why Is A Pancreatic Cancer Diagnosis . . . . So Death Shattering!!!
Why Is A Pancreatic Cancer Diagnosis . . . . So Death Shattering!!!
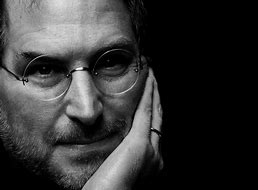
One of the first person I met on Facebook when I started social media — to meet cancer survivors was Lene Maria Søndermølle Steffensen from Denmark. When she told me she survived the same type of cancer Steve Jobs as she prevailed with a Winning Outlook on Life after doing the research. One of the things that I quickly learned about — Lene Maria lead the same type of stress in her life as Steve Jobs. I remember to this day when I heard Steve Jobs transition over. A Computer Turd told me. . .who wanted $150 @ hour to help with the start up of this blog. As I told him–I will learn it on my own in our two minute phone conference. 
Steve Jobs’ “magical thinking” may have defined his business brilliance, but it could have been his downfall in his fight against cancer. When Steve Jobs tumor was detected in 2003 it was diagnosed as locally advanced pancreatic cancer. Although cancer of the pancreas has a terrible prognosis—half of all patients. . . with locally advanced pancreatic cancer die within ten months of the diagnosis; half of those whom it has metastasized – die within six months—cancer in the pancreas is not necessarily a death sentence. Jobs was criticized for putting off surgery 9 months while he sought Alternative Treatment, however, Steve lived until Oct 05, 2011 (age 56).
All the other neuroendocrine tumors have got poor life expectancy with a survival rate at 3 and 5 years nearly found to be equal to 60% and 40% respectively [1]. In comparison, to the exocrine pancreatic tumors, these tumors are known to have a good success rate in their treatment because of lower spreading potential and slower growth rate. In general, if the tumor is detected early on. . . .life expectancy is as high as 10-15 years with regular check-ups and mild dosages of chemotherapy to keep it from recurring. However, if the nerve cells are already affected, like in metastatic pancreatic NET, the life expectancy can go down to as little as 23 months. What causes pancreatic cancer?
KATIE COURIC — fought off the painful memory of her husband’s death from cancer 3 1/2 years ago to bravely support her sister Emily as she succumbed to the same killer disease.
But after 54-year-old Emily Couric’s death from pancreatic cancer on October 18, the “Today Show” host collapsed in tears and had to be virtually carried out of a Virginia funeral home by her nephew.
“Katie sobbed, ‘I’m going to miss her. We all wish we could have done more. But Mother knew how much we all loved her.’ “
Katie, 44, was at her older sister’s side when she died at her home in Charlottesville, Va., as was Emily’s entire family — her husband of 20 years, Dr. George Beller, her parents John and Elinor, brother John Jr., sister Clara Couric Batchelor, two sons and three stepchildren.
“Emily died the way she wanted — with all her loved ones around her,” a source declared.
“And Katie was a rock the last few days and hours.”
For three nights, Katie slept on a cot beside her stricken sister, ministering to her needs in her last hours, said a family friend.
“Katie held Emily’s hand, wiped the sweat from her brow and told her how much she loved her.
“Katie was there when they gave Emily morphine for the pain and when they fed her intravenously. She helped drive away the fear she sometimes saw in her sister’s eyes, whispering words of love and encouragement — even though her heart was breaking.”
In the last days as Katie sat at her bedside, Emily reversed roles and offered Katie encouragement, said the family friend.
She urged Katie — whose husband Jay Monahan also died of colon cancer at age 42 in January 1998 — to wed TV executive Tom Werner, Katie’s boyfriend for more than a year.
Werner filed for divorce from his wife of 28 years last October. “Despite her pain, Emily’s thoughts were for Katie’s future,” the friend revealed.
“She told Katie that she needed to go on with her life, and if she truly loved the man in her life, she should marry him.
“Tom was one of the first people to call Katie to offer sympathy after Emily’s death. When she heard his voice, Katie broke down.
“She told him, ‘My heart’s been broken for a second time. But I’ve got to be strong for the sake of my parents, for my own daughters.’ “
Emily, a Virginia state senator since 1996, was so popular and highly respected in Virginia that it was widely believed she would one day become the state’s first woman governor.
On October 22, Katie celebrated her sister in a moving eulogy at a public service at St. Paul’s Memorial Church in Charlottesville, attended by 2,000 people — including her co-host Matt Lauer.
Katie fought back tears several times during her tribute. Twice she had to stop and drink from a glass of water to compose herself. And she made an emotional reference to her beloved Jay’s passing.
“When my husband died,” said Katie, her voice cracking, “Emily decided to act,” and Virginia became the first state in the nation to pay for color cancer screening tests.
“I can’t think of a better tribute to Jay and now a lasting tribute to her. She taught me not about dying, but about living.”
Fact: women and men share similar chances of getting pancreatic cancer. According to statistics from the American Cancer Society, the average lifetime risk of pancreatic cancer for men is about 1 in 63. For women, the lifetime risk is about 1 in 65.
Pancreatic cancer: Here’s why it’s so deadly!!!
By Elizabeth Landau, CNN 2 days ago
Pancreatic cancer was the third-leading cause of death from cancer in the United States in 2018, after lung and colorectal cancers, according to the National Cancer Institute. This year, an estimated 56,770 new cases of pancreatic cancer will be diagnosed and an estimated 45,750 deaths from pancreatic cancer will occur across the nation, according to the American Cancer Society. About 95% of people with pancreatic cancer die from it, experts say. It’s so lethal because during the early stages, when the tumor would be most treatable, there are usually no symptoms. It tends to be discovered at advanced stages when abdominal pain or jaundice may result. Presently, there are no general screening tools.
As people age, the risk of developing pancreatic cancer goes up. Most patients are older than 45, and nearly 90% are older than 55. The average age at diagnosis is 71. Men have a slightly higher likelihood of developing pancreatic cancer than women, which may partly result from increased tobacco use in men. In the past, when men more commonly smoked than women, the gender gap was wider. Currently, the lifetime risk of developing it is about 1 in 63 for men and 1 in 65 for women. There is also a noted association with race: African-Americans are more likely to develop pancreatic cancer than whites. Doctors don’t know why but speculate that higher rates of men smoking and having diabetes, and women being overweight, may contribute to that association.
What are the types of pancreatic cancer?
The pancreas is an oblong organ that lies deep in the abdomen and is an integral part of both the digestive and endocrine system. It secretes hormones to regulate the body and digestive enzymes to break down food. There are two types of pancreatic cancer: exocrine tumors and endocrine tumors. Exocrine tumors are the majority of pancreatic cancers, and the most common form is called adenocarcinoma, which begins in gland cells, usually in the ducts of the pancreas. These tumors tend to be more aggressive than neuroendocrine tumors, the kind that Apple Inc. co-founder Steve Jobs had, but if caught early enough, they can be treated effectively with surgery.
Pancreatic neuroendocrine tumors constitute only 1% of all pancreatic cancers. They can be benign or malignant, but the distinction is often unclear and sometimes apparent only when the cancer has spread beyond the pancreas. The five-year survival rate for neuroendocrine tumors can range from 50% to 80%, compared with less than 5% for adenocarcinoma. More advanced tumors have a higher risk of recurrence and can spread to the liver, said Dr. Steven Libutti, pancreatic cancer expert and director of the Montefiore-Einstein Center for Cancer Care in the Bronx.
Treatment 0ptions:
Pancreatic cancer is usually controllable only through removal by surgery and only if found before it has spread, according to the National Cancer Institute. Palliative care can help a patient’s quality of life if the disease has spread. Two drugs approved in 2011 may help patients with pancreatic neuroendocrine tumors. They are believed to suppress the blood supply and metabolism of the tumor cells. That’s good progress since, the year before, the standard of care was chemotherapy, said Dr. Michaela Banck, medical oncologist at the Mayo Clinic, who treats patients with neuroendocrine tumors.
Everolimus, marketed by Novartis as Afinitor, received United States FDA approval to treat pancreatic neuroendocrine tumors and prevents transplant rejection. Potential side effects are serious, lung or breathing problems, infections and renal failure, which may lead to death. Sunitinib malate, marketed by Pfizer as Sutent, is prescribed for treatment of pancreatic neuroendocrine tumors, as well as kidney cancer and GIST, a rare cancer of the bowel, esophagus or stomach. Also with everolimus, there are risks to consider: It can cause liver problems and death.
Steve Jobs underwent surgery to remove his tumor in 2004 and died in 2011. His seven-year survival after treatment is consistent with the average survival for these kinds of tumors, Libutti said.
If pancreatic cancers are detected early, that may increase the odds of survival, but it depends on how aggressive the particular tumors are in a patient. If surgery leaves behind microscopic aggressive tumor cells, they can also cause a recurrence of cancer. Steve Jobs underwent a liver transplant in Tennessee in 2009, which is “cutting-edge stuff” for when neuroendocrine tumors spread, said Dr. Maged Rizk, director of the Chronic Abdominal Pain Center at the Cleveland Clinic who specializes in gastroenterology and hepatology.
Do Transplants Help?
Because it’s so rare, there isn’t a lot of evidence to support the transplant as a cure; the procedure could extend life, but also, immunosuppression drugs may allow any remaining cancer to grow faster, doctors say. And a European study found the majority of patients who underwent liver transplant for this type of tumor had recurrence of the disease. But many pancreatic cancers are detected in later stages because when the tumor is small, it often does not produce symptoms. As they grow, adenocarcinomas can obstruct the ducts from the liver and cause severe back pain. Neuroendocrine tumors sometimes produce insulin, so a patient’s first symptoms could be low glucose levels. But most tumors do not produce hormones, Libutti said.
There are two rare genetic syndromes — multiple endocrine neoplasia type 1 (MEN1) and Von Hippel-Lindau syndrome (VHL) — that increase the risk of pancreatic neuroendocrine tumors. Other than that, although, it maybe unclear whether having a family member with pancreatic cancer increases an individual’s risk. Pancreatic cancer struck former President Jimmy Carter’s family hard. He lost his father — also all of his siblings, brother Billy and sisters Ruth Carter Stapleton and Gloria Carter Spann.
The Future of Treatment
Researchers are working on better understanding the way in which pancreatic tumors grow and spread, Libutti said. There’s a lot research focused on finding better treatments, targeted therapies, immune therapy, improving surgery and radiation therapy, according to the American Cancer Society. “There are a number of agents that are being looked at in clinical trials that focus on pathways that may allow pancreatic cancer to evade normal processes,” Libutti said.
Another line of research is focused on finding biomarkers of pancreatic cancer so that a simple blood or urine test could be developed. Unlike screenings for other conditions such as colon, breast and prostate cancers, there is no routine way to see whether a patient has a tumor in the pancreas. The future of medicine to help people with pancreatic cancer will involve genetics, Banck said. This would involve. . . matching a person’s particular type of tumor using genomic information with treatment. “What’s going to make real differences in the future to surviving pancreatic cancer is the revolution of the genomic era.”
Pancreatic cancer: Cannabis compound may boost survival.
Cancer patients have reported finding relief from pain and stimulation of appetite from the use of medical marijuana, also known as cannabis. In fact, Patient Central at the Pancreatic Cancer Action Network (PanCAN), which provides free, in-depth and personalized resources and information about pancreatic cancer, has received many questions about the use and effects of medical marijuana. For example, how is marijuana derived and how can it be used by cancer patients?
Marijuana is a plant that contains substances called cannabinoids. The cannabinoids found in marijuana plants may help treat the symptoms and the side effects caused by cancer and cancer treatments. In addition. . . .to the naturally occurring cannabinoids found in marijuana plants and how it helps pancreatic cancer.
The use of marijuana and cannabinoid drugs for medicinal purposes, such as controlling pain and stimulating appetite in cancer patients, have been and continue to be studied in the lab and in clinics. Consequently, conflicting information has been reported in clinical studies using cannabinoids as pain relievers or appetite stimulants for cancer survivors.
Some studies have reported that patients regained appetites and sense of taste, while others reported cannabinoids are no more helpful. . . than other prescription appetite stimulant medications. Likewise, some studies about pain relief also report promising results, while others have shown cannabinoids are no more helpful than prescription medications for controlling pain.
Its important for patients to speak with their doctor to determine if marijuana would be helpful in their fight against pancreatic cancer. According to Victoria Manax, MD, PanCAN’s Chief Medical Officer, “Since there has not been sufficient data generated yet to produce consistent clinical results about the benefits of medical marijuana for patients, we encourage patients to discuss problems ( pain and appetite stimulation) with their doctor to determine the right medications to help control such issues.”
Patient Central often receives questions about how medical marijuana can be used when fighting pancreatic cancer. Here are five things to know:
What is marijuana? Marijuana is a plant grown in many parts of the world which produces resin containing compounds called cannabinoids. Some cannabinoids are psychoactive, meaning they act on the brain to change mood or consciousness.
In which states is medical marijuana legal? More than 30 states have some type of legal medical marijuana program. Find out if it is legal in your state.
What are the active ingredients? The main active cannabinoid in marijuana is delta-9-THC. Another active cannabinoid is cannabidiol (CBD), which may relieve pain, lower inflammation, and decrease anxiety without causing the “high” of delta-9-THC.
How can medical marijuana be administered? Cannabinoids are available in a variety of formats. They can be taken by mouth as capsules, sprayed under the tongue, included as an ingredient in food and eaten, inhaled, or used topically.
Has the FDA approved marijuana for cancer use? Two cannabinoids (dronabinol and nabilone) are drugs approved by the U.S. Food and Drug Administration (FDA) for the prevention or treatment of chemotherapy-related nausea and vomiting. Pancreatic Cancer Cannabis Survivor Stories!!!

