The Man Who Can Solve 41 Rubik’s Cubes—
Marcin “Maskow” Kowalczyk is a speed-cuber. That means he can solve a Rubik’s Cube very quickly. Oh yeah …. he can do it while blindfolded. Has Advice For Doing Amazing Things With Your Brain !!!!!
Lack of sleep can rob your brain of the skills required to successfully navigate life, and new research has added another impairment to the list. In this study (described here), https://www.sciencedaily.com/releases/2017/03/170323132524.htm people deprived of sleep for a night had trouble identifying a facial expression as happy or sad. That’s on top of the purely cognitive impairments that sleep deprivation can bring. We frequently discuss how sleep issues lead to brain issues, and we will have more to say as we analyze the results of The World’s Largest Sleep Study. The authors speculate this could affect everyday social interactions. Misreading a spouse or co-worker as happy when they are actually sad could cause an inappropriate response, putting a strain on relationships.
The Treatable Disease That’s Misdiagnosed as Alzheimer’s.
It tends to strike older Americans, causing memory loss, difficulty walking, and other symptoms that lead many doctors to misdiagnose it as dementia or Alzheimer’s disease.
But experts say up to 5 % of Americans diagnosed with those incurable brain disorders actually have a treatable condition called “normal pressure hydrocephalus.”
Many of the estimated 375,000 Americans who have NPH don’t even know it, because its symptoms are strikingly similar to dementia, mental-health specialists say. As a result, thousands of NPH patients never benefit from surgical procedures that can miraculously correct and reverse the condition.
Gary Small, M.D., a University of California-Los Angeles professor of psychiatry and aging, tells Newsmax Health that NPH can be detected by MRI or CT scans of the brain that help patients get the help they need. But doctors never order such tests for untold numbers of Americans with NPH.
“What can happen, and I’m not sure how frequent this misdiagnosis occurs, is people go in to their doctor with what look like dementia, or Alzheimer’s symptoms or even Parkinson’s — memory problems, and this unsteady gait, and incontinence,” says Dr. Small, director of the Longevity Center and author of The Alzheimer’s Prevention Program.
“The doctor may think it looks like so many of my other [dementia] cases that I’m not going to bother to have a scan.” The condition, which is caused by a buildup of fluid in the brain, is rare and was only discovered in the 1960s, which may explain why it is frequently missed or misdiagnosed.
“In my 30 years of practice, I’ve seen at most three to four cases, so it’s not that common,” notes Dr. Small, author of The Mind Health Report newsletter. “But we always look for it and [doctors should] always check for it.”
NPH has received an increased dose of media attention recently, but still remains under the radar for many doctors and patients.
According to the Hydrocephalus Foundation, NPH occurs when the brain’s natural system for draining and absorbing cerebrospinal fluid malfunctions. The cavities in the brain — known as ventricles — enlarge and fill with extra fluid and put pressure on areas of the brain that control the movement, bladder functions, and mental processes such as memory, reasoning, problem solving, and speaking .
What causes NPH is unknown, but experts say it typically occurs after a head injury, stroke, meningitis, brain cancer, or surgery. Most people with NPH are diagnosed after age 60. In addition to memory loss and a decline in mental processes (similar to Alzheimer’s), NPH typically can causes difficulty walking (like Parkinson’s) and urinary incontinence. It can also cause speech problems, changes in mood and behavior, headache, nausea, and vision problems.
What causes Parkinson disease?
Parkinson disease arises from decreased dopamine production in the brain. The absence of dopamine makes it hard for the brain to coordinate muscle movements. Low dopamine also contributes to mood and cognitive problems later in the course of the disease. Experts don’t know what triggers the development of Parkinson disease. As early onset Parkinson disease is often inherited and is the result of certain gene defects.
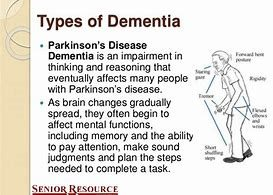
Experts don’t understand how or why dementia often occurs with Parkinson disease. It’s clear, though, dementia and problems with cognitive function are linked to changes in the brain that cause problems with movement. As with Parkinson disease, dementia occurs when nerve cells degenerate, leading to chemical changes in the brain. Parkinson disease dementia may be treated with medicines also used to treat Alzheimer’s disease, another type of dementia.
The Hydrocephalus Association estimates about 5 percent of Americans diagnosed with dementia actually have NPH, with a total of 375,000 cases in the U.S. But that figure is expected to grow as the population ages. The good news is that NPH, unlike Alzheimer’s and Parkinson’s — can be treated and its symptoms reversed, but only if it is diagnosed correctly, Dr. Small notes. Brain scans can identify the hallmark signs of NPH — dilated ventricles in the brain that fill with cerebrospinal fluid.
“If you see what look like dilated ventricles, it suggests concern [for NPH],” he explains. “Those ventricles surround that fluid in the brain. Hydrocephalus means ‘water on the brain.’ ” NPH can be treated through surgery, during which a shunt — a thin tube — is implanted in the brain by a neurosurgeon to drain excess fluid.
The tube is threaded under the skin from the head to another part of the body, usually the belly. A valve can be opened to release the fluid when the pressure builds up. The fluid drains harmlessly and is absorbed by the bloodstream. Although a shunt operation won’t cure the underlying cause of NPH, it can relieve the symptoms.
Shunt operations don’t work for everyone, but the Hydrocephalus Association reports many patients report miraculously regaining their ability to remember, walk, talk, and control their physical and mental abilities. The earlier the NPH is diagnosed, the better the odds a patient will benefit from surgery.
“If it’s recognized early you have the opportunity to intervene and have the benefit of that intervention, and release the pressure surgically,” Dr. Small says. “Neurosurgeons have a way of testing to see if surgery will help.”
A widely publicized study of NPH suggests almost one-third of American physicians have never even heard of NPH. Harold Conn, M.D., a retired Yale University professor, was diagnosed with NPH 10 years ago after mistakenly being told by his doctors that he had Parkinson’s. After recovering he surveyed 166 doctors and found 30 percent were completely unaware of NPH. Most graduated from medical school before NPH was first described in medical literature in 1965.
Dr. Small says the upshot is that family members of individuals with symptoms of dementia should be aware that they may actually be suffering from NPH or other conditions that are treatable.
“What’s important is people need to know if they’re having memory problems or a cognitive decline — even though Alzheimer’s is the leading cause of these things — there are a lot of other things that can cause these symptoms,” he notes.
“It could be NPH, depression, a thyroid imbalance, anemia. Even a drug toxicity, a sleeping medicine, or medicine that interacts badly with other medicines [can] cause this. And sometimes some of these causes are reversible.”
Dementia is an umbrella term for a group of symptoms caused by disorders that affect the brain, including devastating diseases like the most common form of dementia, Alzheimer’s disease and lesser-known forms of dementia like Lewy body dementia. Even stroke can cause dementia.
More than 5 million people in the U.S. alone are living with Alzheimer’s, so there’s a good chance you know someone affected by dementia. It can be very difficult to watch someone you love deal with – symptoms of dementia, which often includes memory loss and trouble with language, along with personality changes, delusions, agitation and less ability to solve problems or control their emotions. It’s also important to note that although dementia risk increases with age, it is not part of the normal aging process.
With comprehensive treatments on the horizon, we can feel hopeful that integrative, personalized approaches could be the key to fighting this disease. In the meantime, though, it’s important you take relatively simple steps to lower your risk of dementia now — before the disease has a chance to set in.
Tune in now to hear about some unexpected causes of dementia and how small lifestyle changes you make today can naturally prevent dementia later in life! https://www.alz.org/facts/
Simple Ways to Help Someone Living With Dementia!!!
“Reminiscence therapy” helps trigger dementia patients’ memories.
Reversing Alzheimers & Dementia Through Stress Management!!!
Additional research shows that anxiety may actually decreases in the severe stages of dementia. When anxiety is present with dementia, it is associated with poor quality of life and behavioral disturbances, even after controlling for depression.
Doctors help you with trusted information about Difficulty Walking in Dementia:
Dr. Daniel G.Krauser on dementia and walking problems: Walking is a complex process, and many different medical problems can affect it. To walk talk & laugh helps your brain to stay active.
There is no known way to prevent Alzheimer’s disease and other related dementias. However, there are actions that one can take to reduce the risk for dementia and, in some cases, slow the progression of the disease.
Recent research is proving that the progression of Alzheimer’s disease and dementia are linked to something called oxidative stress. Oxidative stress is caused by a combination of poor lifestyle choices and a diet that produces increased levels of oxidative radicals and lower levels of antioxidants. A diet that reverses oxidative stress and Ways to prevent & reverse cognitive decline are:

Healthy Diet (coconut oil.) Omega 3s and B Vitamin’s
Heart Healthy Behaviors
Avoiding Head Injury
Physical Exercise Mental Activity
Socializing….
Some factors may decrease the effect of brain damage due to dementia by developing more connections between the remaining brain cells, rather than preventing damage. With more connections between brain cells, function can be maintained longer despite damage to the brain.
Slight changes in the way a person walks, like slowing down or developing a variable -stride, could be early signs of Alzheimer’s disease. Previous studies have linked walking speed in the elderly with overall good health & even longevity, with the current research among the first to associate gait with risk of Alzheimer’s. The 4 new studies, presented over the weekend at the Alzheimer’s Association International Conference in Vancouver, find that changes in physical movements like walking can even precede symptoms of cognitive decline.
One study by researchers at the Basel Mobility Center in Switzerland followed 1,153 elderly participants including patients at the center being treated for memory & mobility problems as well as volunteers in a separate 2007-11 cohort study. The participants were separated into groups based on their cognitive status: cognitively healthy, diagnosed with mild cognitive impairment (MCI) or diagnosed with Alzheimer’s dementia.
Researchers tested participants’ gait on a 33-ft. electronic walkway containing 30,000 integrated pressure sensors. The participants were tested for “normal” walking and for performance on two “dual tasks,” which included normal walking while simultaneously counting backward out loud or while naming animals.
When people are asked to walk and perform a cognitive task at the same time, these regions of the brain become overloaded because they have to share the resources between the two tasks. In people who are cognitively impaired, these networks become increasingly overloaded due to having less cognitive reserve. Thus, the amount of gait slowing a person exhibits while performing a dual-task gait test, compared with his or her usual gait velocity (without a cognitive task) provides a measure of the person’s deficits in executive function, attention, and memory processes.
This magnitude of gait slowing can be expressed as a dual-task gait cost, which adjusts for the individual’s own usual walking characteristics. In one recent study, they examined the association of dual-task gait performance and the incidence of dementia in people with MCI. These participants were followed for six years as part of the Gait and Brain Study, an ongoing study (clinicaltrials.gov identifier: NTC03020381) designed to determine whether gait deficits can predict cognitive and mobility decline and progression to dementia among community-dwelling older adults.
Overall, everyone walked slower while attempting to multitask, however, walking speed was also linked with people’s varying levels of cognitive decline. People with Alzheimer’s walked slower than those with MCI, who walked slower than cognitively healthy adults ”Mobility impairments are often associated with dementia, and some gait changes may even appear before cognitive decline can be detected by traditional testing methods,” said lead study author Dr. Stephanie Bridenbaugh in a statement. “Gait analysis can simply, quickly and objectively measure walking. When problems emerge, this may provide early detection of fall risk and the earliest stages of cognitive impairment in older adults.”
Dr. Joe Verghese has found that nearly in 1 in 10 older adults met criteria for pre-dementia based on a simple test measuring how fast people walk and to whether they have cognitive complaints. People who tested positive for this pre-dementia were twice as likely as others to develop dementia within twelve years.
In this extended version, Dr. Verghese gives specific walking speeds that are considered unusually slow and explains why those with vascular disease, diabetes or high blood p.s.i., pressure are at increased risk for dementia. The paper was published online on July 16 in Neurology. Dr. Verghese is professor of neurology and medicine at Albert Einstein College of Medicine and chief of geriatrics at Einstein and Montefiore Medical Center.
Walking may slow the cognitive decline in adults with Alzheimer’s disease, according to a new study presented Monday at the annual meeting of the Radiological Society of North America.
The study, done by Cyrus Raji at the University of Pittsburgh, found that walking about eight kilometres per week helped to slow memory loss.
“We found that walking . . . protects the brain structure over 10 years in people with Alzheimer’s and MCI, (mild cognitive impairment) especially in areas of the brain’s key memory and learning centres,” said Raji. “We also found that these people had a slower decline in memory loss over five years.”
Alzheimer’s is an incurable brain disease that destroys memory and cognitive skills. According to the Alzheimer’s Society of Canada, there were about 480,000 Canadians with Alzheimer’s and related dementia in 2008. The society estimates that number will reach 1,125,200 by 2038.
The society also estimates the economic burden of dementia in Canada doubles every decade, increasing from $15 billion in 2008 to $153 billion in 2038.
“Because a cure for Alzheimer’s is not yet a reality, we hope to find ways of alleviating disease progression or symptoms in people who are already cognitively impaired,” Raji said.
For the ongoing study, Raji and his colleagues analyzed the relationship between physical activity and brain structure in 426 people, including 299 healthy adults (average age 78), and 127 cognitively impaired adults (average age 81), including 83 adults with MCI and 44 adults with Alzheimer’s dementia.
The study looked at how far patients walked in a week. After 10 years, all subjects underwent MRI exams to identify brain volume changes.
“Volume is a vital sign for the brain,” Raji said. “When it decreases, that means brain cells are dying. But when it remains higher, brain health is being maintained.”
Subjects were also given mental state exams to track cognitive decline over five years. Physical activity levels were correlated with the exam and MRI results.
Raji said the findings showed that greater amounts of physical activity were associated with greater brain volume.
“Cognitively impaired people needed to walk at least 58 city blocks, or approximately 5 miles (eight kilometres), per week, to maintain brain volume and slow cognitive decline. The healthy adults needed to walk at least 72 city blocks, or six miles, per week maintain brain volume and significantly reduce their risk for cognitive decline,” Raji said in a release Monday.
“Alzheimer’s is a devastating illness, and unfortunately, walking is not a cure, “Raji said. “But walking can improve your brain’s resistance to the disease and reduce memory loss over time.”
The Alzheimer’s Society of Canada, in its Rising Tide report, urges a national dementia strategy be adopted in Canada which would include recognizing the importance of informal caregivers and an increase in all areas of dementia research.
Compared to Alzheimer’s disease, which happens when the brain’s nerve cells break down, vascular dementia happens when part of the brain doesn’t get enough blood carrying the oxygen and nutrients it needs. What are the symptoms of vascular dementia?
Not all patients who suffer from dementia or Alzheimer’s will exhibit Sundowner’s, however. Conversely, some people exhibit symptoms of dementia all day which grow worse in the late afternoon and evening, while others may exhibit no symptoms at all until the sun goes down.Sundowner’s Syndrome largely remains a mystery to medical science, although there are several theories about why these symptoms begin at night. More and more studies are being conducted to try to determine the exact cause.
In the meantime, some doctors believe it’s an accumulation of all of the sensory stimulation from the day which begins to overwhelm and cause stress. Some speculate that Sundowner’s Syndrome is caused by hormonal imbalances that occur at night. Still others believe that the onset of symptoms at night is due to simple fatigue, while some believe it has to do with the anxiety caused by the inability to see as well in the dark.
https://www.unforgettable.org/blog/coping-with-unresponsiveness-and-apathy-in-someone-with-dementia/?fbclid=IwAR17GPGvDj5ciD4_vfx-FjRMaE_hXrlOb8Yh8UtqUtV5peL4eEZEXo8rmbU
How to Prevent Dementia Patients from Wandering … Create a circular walking trail. People with dementia often suffer from stress and fear, and those feelings may prompt them to wander in order to calm themselves down, according to the Mayo Clinic.
Walking may slow cognitive decline in adults with mild cognitive impairment (MCI) and Alzheimer’s disease, as well as in healthy adults, according to a study presented November 29 at the meeting of the Radiological Society of North America (RSNA).
“We found that walking five miles per week protects the brain structure over 10 years in people with Alzheimer’s and MCI, especially in areas of the brain’s key memory & learning centers,” said Cyrus Raji, Ph.D., from the Department of Radiology at the University of Pittsburgh in Pennsylvania. “We found that these people had a slower decline in memory loss over five years.”
Alzheimer’s disease is an irreversible, progressive brain disease that slowly destroys memory and cognitive skills. According to the National Institute on Aging, between 2.4 million and 5.1 million Americans have Alzheimer’s disease. Based on current population trends, that number will increase significantly over the next decade.